Atrial flutter is a cardiac arrhythmia characterized by atrial rates of 240-400 beats/min and some degree of atrioventricular (AV) node conduction block. For the most part, morbidity and mortality are due to complications of rate (eg, syncope and congestive heart failure [CHF]).
Essential update: Catheter ablation successfully treats scar-related atypical atrial flutterWith the aid of a combination of high-density activation and entrainment mapping, catheter ablation can be successfully used to treat scar-related atypical atrial flutter or atrial tachycardia, according to a report by Coffey et al.[1] The retrospective investigation also found that the highest rates of acute and long-term recurrences of atrial tachycardia were in patients with the septal form of the condition.
The study involved 91 consecutive patients with a total of 171 atrial tachycardias.[1] Irrigated radiofrequency ablation (RFA) of constrained areas along the circuit produced acute success rates of 97% for patients with nonseptal atrial tachycardia and 77% and those with septal atrial tachycardia. Long-term success rates were 82% for patients with nonseptal atrial tachycardia and 67% for those with at least 1 septal atrial tachycardia.
In patients whose atrial tachycardia was associated with previous catheter ablation, cardiac surgery or a maze procedure, or idiopathic atrial scarring, the long-term success rates were 75%, 88%, and 57%, respectively.[1]
Signs and symptomsSigns and symptoms in patients with atrial flutter typically reflect decreased cardiac output as a result of the rapid ventricular rate. Typical symptoms include the following:
PalpitationsFatigue or poor exercise toleranceMild dyspneaPresyncopeLess common symptoms include angina, profound dyspnea, or syncope. Tachycardia may or may not be present, depending on the degree of AV block associated with the atrial flutter activity.
Physical findings include the following:
The heart rate is often approximately 150 beats/min because of a 2:1 AV blockThe pulse may be regular or slightly irregularHypotension is possible, but normal blood pressure is more commonly observedOther points in the physical examination are as follows:
Palpate the neck and thyroid gland for goiterEvaluate the neck for jugular venous distentionAuscultate the lungs for rales or cracklesAuscultate the heart for extra heart sounds and murmursPalpate the point of maximum impulse on the chest wallAssess the lower extremities for edema or impaired perfusionIf embolization has occurred from intermittent atrial flutter, findings are related to brain or peripheral vascular involvement. Other complications of atrial flutter may include the following:
CHFSevere bradycardiaMyocardial rate–related ischemiaSee Presentation for more detail.
DiagnosisThe following techniques aid in the diagnosis of atrial flutter:
ECG – This is an essential diagnostic modality for this conditionVagal maneuvers – These can be helpful in determining the underlying atrial rhythm if flutter waves are not seen wellAdenosine – This can be helpful in the diagnosis of atrial flutter by transiently blocking the AV nodeExercise testing – This can be utilized to identify exercise-induced atrial fibrillation and to evaluate ischemic heart disease Holter monitor – This can be used to help identify arrhythmias in patients with nonspecific symptoms, to identify triggers, and to detect associated atrial arrhythmiasTransthoracic echocardiography (TTE) is the preferred modality for evaluating atrial flutter. It can evaluate right and left atrial size, as well as the size and function of the right and left ventricles, and this information facilitates diagnosis of valvular heart disease, left ventricular hypertrophy (LVH), and pericardial disease.
See Workup for more detail.
ManagementGeneral treatment goals for symptomatic atrial flutter are similar to those for atrial fibrillation. They include the following:
Control of ventricular rate – This can be achieved with drugs that block the AV node; intravenous (IV) calcium channel blockers (eg, verapamil and diltiazem) or beta blockers can be used, followed by initiation of oral agents Restoration of sinus rhythm – This can be done by means of electrical or pharmacologic cardioversion or RFA; successful ablation reduces or eliminates the need for long-term anticoagulation and antiarrhythmic medications Prevention of recurrent episodes or decrease in their frequency or duration – In general, the use of antiarrhythmic drugs in atrial flutter is similar to that in atrial fibrillation Prevention of thromboembolic complications – Adequate anticoagulation, as recommended by the American College of Chest Physicians, has been shown to decrease thromboembolic complications in patients with chronic atrial flutter and in patients undergoing cardioversion Minimization of adverse effects from therapy – Because atrial flutter is a nonfatal arrhythmia, carefully assess the risks and benefits of drug therapy, especially with antiarrhythmic agentsSee Treatment and Medication for more detail.
Image library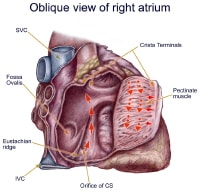 Anatomy of classic counterclockwise atrial flutter. This demonstrates oblique view of right atrium and shows some crucial structures. Isthmus of tissue responsible for atrial flutter is seen anterior to coronary sinus orifice. Eustachian ridge is part of crista terminalis that separates roughened part of right atrium from smooth septal part of right atrium. NextBackground
Anatomy of classic counterclockwise atrial flutter. This demonstrates oblique view of right atrium and shows some crucial structures. Isthmus of tissue responsible for atrial flutter is seen anterior to coronary sinus orifice. Eustachian ridge is part of crista terminalis that separates roughened part of right atrium from smooth septal part of right atrium. NextBackgroundAtrial flutter is a cardiac arrhythmia characterized by atrial rates of 240-400 beats/min, usually with some degree of atrioventricular (AV) node conduction block. In the most common form of atrial flutter (type I atrial flutter), electrocardiography (ECG) demonstrates a negative sawtooth pattern in leads II, III, and aVF.
Type I (typical or classic) atrial flutter involves a single reentrant circuit with circus activation in the right atrium around the tricuspid valve annulus. The circuit most often travels in a counterclockwise direction. Type II (atypical) atrial flutter follows a different circuit; it may involve the right or the left atrium. (See Pathophysiology.)
Atrial flutter is associated with a variety of cardiac disorders. In most studies, approximately 60% of patients with atrial flutter have coronary artery disease (CAD) or hypertensive heart disease; 30% have no underlying cardiac disease. Uncommon forms of atrial flutter have been noted during long-term follow-up in as many as 26% of patients with surgical correction of congenital cardiac anomalies. (See Etiology.)
Symptoms in patients with atrial flutter typically reflect decreased cardiac output as a result of the rapid ventricular rate. The most common symptom is palpitations. Other symptoms include fatigue, dyspnea, and chest pain. (See Presentation.) ECG is essential in making the diagnosis. Transthoracic echocardiography (TTE) is the preferred modality for evaluating atrial flutter. (See Workup.)
Intervening to control the ventricular response rate or to return the patient to sinus rhythm is important. Consider immediate electrical cardioversion for patients who are hemodynamically unstable. Consider catheter-based ablation as first-line therapy in patients with type I typical atrial flutter if they are reasonable candidates. Ablation is usually done as an elective procedure; however, it can also be done when the patient is in atrial flutter. (See Treatment.)
Atrial flutter is similar to atrial fibrillation in many respects (eg, underlying disease, predisposing factors, complications, and medical management), and some patients have both atrial flutter and atrial fibrillation. However, the underlying mechanism of atrial flutter makes this arrhythmia amenable to cure with percutaneous catheter-based techniques.
PreviousNextPathophysiologyIn humans, the most common form of atrial flutter (type I) involves a single reentrant circuit with circus activation in the right atrium around the tricuspid valve annulus (most often in a counterclockwise direction), with an area of slow conduction located between the tricuspid valve annulus and the coronary sinus ostium (subeustachian isthmus). A 3-dimensional electroanatomic map of type I atrial flutter is shown in the video below.
3-Dimensional electroanatomic map of type I atrial flutter. Colors progress from blue to red to white and represent relative conduction time in right atrium (early to late). Ablation line (red dots) has been created on tricuspid ridge extending to inferior vena cava. This interrupts flutter circuit. RAA = right atrial appendage; CSO = coronary sinus os; IVC = inferior vena cava; TV = tricuspid valve annulus.Animal models have been used to demonstrate that an anatomic block (surgically created) or a functional block of conduction between the superior vena cava and the inferior vena cava, similar to the crista terminalis in the human right atrium, is key to initiating and maintaining the arrhythmia.
The crista terminalis acts as another anatomic conduction barrier, similar to the line of conduction block between the 2 venae cavae required in the animal model. The orifices of both venae cavae, the eustachian ridge, the coronary sinus orifice, and the tricuspid annulus complete the barrier for the reentry circuit (see the image below). Type I atrial flutter is often referred to as isthmus-dependent flutter. Usually, the rhythm is due to reentry, there is an excitable gap, and the rhythm can be entrained.
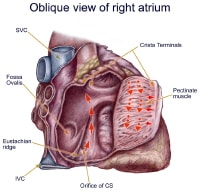 Anatomy of classic counterclockwise atrial flutter. This demonstrates oblique view of right atrium and shows some crucial structures. Isthmus of tissue responsible for atrial flutter is seen anterior to coronary sinus orifice. Eustachian ridge is part of crista terminalis that separates roughened part of right atrium from smooth septal part of right atrium.
Anatomy of classic counterclockwise atrial flutter. This demonstrates oblique view of right atrium and shows some crucial structures. Isthmus of tissue responsible for atrial flutter is seen anterior to coronary sinus orifice. Eustachian ridge is part of crista terminalis that separates roughened part of right atrium from smooth septal part of right atrium. Type I counterclockwise atrial flutter has caudocranial activation (ie, activation counterclockwise around the tricuspid valve annulus when viewed in the left antero-oblique fluoroscopic view) of the atrial septum (see the image below).
 Type I counterclockwise atrial flutter. This 3-dimensional electroanatomic map of tricuspid valve and right atrium shows activation pattern displayed in color format. Red is early and blue is late, relative to fixed point in time. Activation travels in counterclockwise direction.
Type I counterclockwise atrial flutter. This 3-dimensional electroanatomic map of tricuspid valve and right atrium shows activation pattern displayed in color format. Red is early and blue is late, relative to fixed point in time. Activation travels in counterclockwise direction. Type I atrial flutter can also have the opposite activation sequence (ie, clockwise activation around the tricuspid valve annulus). Clockwise atrial flutter is much less common. When the electric activity moves in a clockwise direction, the ECG will show positive flutter waves in leads II, III, and aVF and may appear somewhat sinusoidal. This arrhythmia is still considered type I, isthmus-dependent flutter; it is usually called reverse typical atrial flutter.
Type II (atypical) atrial flutters are less extensively studied and electroanatomically characterized. Atypical atrial flutters may originate from the right atrium, as a result of surgical scars (ie, incisional reentry), or from the left atrium, specifically the pulmonary veins (ie, focal reentry) or mitral annulus (see the image below). Left atrial flutter is common after incomplete left atrial linear ablation procedures (for atrial fibrillation). Thus, tricuspid isthmus dependency is not a prerequisite for type II atrial flutter.
 Atypical left atrial flutter. PreviousNext, Atrial Flutter
Atypical left atrial flutter. PreviousNext, Atrial Flutter






What cardiology equipment companies have the best ECG machines? Do you think it's worth checking online medical device directory or it's better to buy straight from developers? Thank you for your answer.
ReplyDeleteNice article.
ReplyDeleteI believe Atrial flutter is a cardiac arrhythmia characterized by atrial rates of 240-400 beats/min, usually with some degree of atrioventricular (AV) node conduction block.