Hypertension affects approximately 75 million adults in the United States and is a major risk factor for stroke, myocardial infarction, vascular disease, and chronic kidney disease.
Essential update: A better model for predicting the development of hypertensionIn an analysis of 4,388 patients enrolled in the Coronary Artery Risk Development in Young Adults (CARDIA) study, a prediction model based on Framingham Heart Study criteria was better than prehypertension at identifying young adults who went on to develop new hypertension in the following 25 years. The c index for incident hypertension was 0.84 using the Framingham prediction model and 0.71 using prehypertension.[1, 2]
Criteria used in the CARDIA prediction model included age, sex, body mass index, smoking, systolic blood pressure (BP), and parental history of hypertension. Prehypertension was defined as systolic BP 120-139 mm Hg or diastolic BP 80-89 mm Hg
Signs and symptomsHypertension is defined as a systolic blood pressure (SBP) of 140 mm Hg or more, or a diastolic blood pressure (DBP) of 90 mm Hg or more, or taking antihypertensive medication.[3]
Based on recommendations of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7), the classification of BP for adults aged 18 years or older is as follows[4] :
Normal: Systolic lower than 120 mm Hg, diastolic lower than 80 mm HgPrehypertension: Systolic 120-139 mm Hg, diastolic 80-89 mm HgStage 1: Systolic 140-159 mm Hg, diastolic 90-99 mm HgStage 2: Systolic 160 mm Hg or greater, diastolic 100 mm Hg or greaterHypertension may be primary, which may develop as a result of environmental or genetic causes, or secondary, which has multiple etiologies, including renal, vascular, and endocrine causes. Primary or essential hypertension accounts for 90-95% of adult cases, and secondary hypertension accounts for 2-10% of cases.
See Clinical Presentation for more detail.
DiagnosisThe evaluation of hypertension involves accurately measuring the patient’s blood pressure, performing a focused medical history and physical examination, and obtaining results of routine laboratory studies.[4, 5] A 12-lead electrocardiogram should also be obtained. These steps can help determine the following[4, 5, 6] :
Presence of end-organ diseasePossible causes of hypertensionCardiovascular risk factorsBaseline values for judging biochemical effects of therapyOther studies may be obtained on the basis of clinical findings or in individuals with suspected secondary hypertension and/or evidence of target-organ disease, such as CBC, chest radiograph, uric acid, and urine microalbumin.[4]
See Workup for more detail.
ManagementMany guidelines exist for the management of hypertension. Most groups, including the JNC, the American Diabetes Associate (ADA), and the American Heart Association/American Stroke Association (AHA/ASA) recommend lifestyle modification as the first step in managing hypertension.
Lifestyle modifications
JNC7 recommendations to lower BP and decrease cardiovascular disease risk include the following, with greater results achieved when 2 or more lifestyle modifications are combined[4] :
Weight loss (range of approximate systolic BP reduction [SBP], 5-20 mm Hg per 10 kg)Limit alcohol intake to no more than 1 oz (30 mL) of ethanol per day for men or 0.5 oz (15 mL) of ethanol per day for women and people of lighter weight (range of approximate SBP reduction, 2-4 mm Hg) Reduce sodium intake to no more than 100 mmol/day (2.4 g sodium or 6 g sodium chloride; range of approximate SBP reduction, 2-8 mm Hg)[7] Maintain adequate intake of dietary potassium (approximately 90 mmol/day)Maintain adequate intake of dietary calcium and magnesium for general healthStop smoking and reduce intake of dietary saturated fat and cholesterol for overall cardiovascular healthEngage in aerobic exercise at least 30 minutes daily for most days (range of approximate SBP reduction, 4-9 mm Hg)The AHA/ASA recommends a diet that is low in sodium, is high in potassium, and promotes the consumption of fruits, vegetables, and low-fat dairy products for reducing BP and lowering the risk of stroke. Other recommendations include increasing physical activity (30 minutes or more of moderate intensity activity on a daily basis) and losing weight (for overweight and obese persons).
The 2013 European Society of Hypertension (ESH) and the European Society of Cardiology (ESC) guidelines recommend a low-sodium diet (limited to 5 to 6 g per day) as well as reducing body-mass index (BMI) to 25 kg/m2 and waist circumference (to [8, 9]
Pharmacologic therapy
If lifestyle modifications are insufficient to achieve the goal BP, there are several drug options for treating and managing hypertension. Thiazide diuretics are the preferred agents in the absence of compelling indications.[4]
Compelling indications may include high-risk conditions such as heart failure, ischemic heart disease, chronic kidney disease, and recurrent stroke, or those conditions commonly associated with hypertension, including diabetes and high coronary disease risk. Drug intolerability or contraindications may also be factors.[4] An angiotensin-converting enzyme (ACE) inhibitor, angiotensin receptor blocker (ARB), calcium channel blocker (CCB), and beta-blocker are all acceptable alternative agents in such compelling cases.
The following are drug class recommendations for compelling indications based on various clinical trials[4] :
Heart failure: Diuretic, beta-blocker, ACE inhibitor, ARB, aldosterone antagonistPostmyocardial infarction: Beta-blocker, ACE inhibitor, aldosterone antagonistHigh coronary disease risk: Diuretic, beta-blocker, ACE inhibitor, CCBDiabetes: Diuretic, beta-blocker, ACE inhibitor, ARB, CCBChronic kidney disease: ACE inhibitor, ARBRecurrent stroke prevention: Diuretic, ACE inhibitorSee Treatment and Medication for more detail.
Image library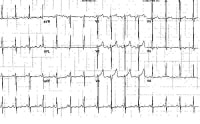 Electrocardiogram (ECG) from a 47-year-old man with a long-standing history of uncontrolled hypertension. This image shows left atrial enlargement and left ventricular hypertrophy. NextBackground
Electrocardiogram (ECG) from a 47-year-old man with a long-standing history of uncontrolled hypertension. This image shows left atrial enlargement and left ventricular hypertrophy. NextBackgroundHypertension is one of the most common worldwide diseases afflicting humans and is a major risk factor for stroke, myocardial infarction, vascular disease, and chronic kidney disease. Despite extensive research over the past several decades, the etiology of most cases of adult hypertension is still unknown, and control of blood pressure is suboptimal in the general population. Due to the associated morbidity and mortality and cost to society, preventing and treating hypertension is an important public health challenge. Fortunately, recent advances and trials in hypertension research are leading to an increased understanding of the pathophysiology of hypertension and the promise for novel pharmacologic and interventional treatments for this widespread disease.
According to the American Heart Association (AHA), approximately 75 million adults in the United States are affected by hypertension, which is defined as a systolic blood pressure (SBP) of 140 mm Hg or more or a diastolic blood pressure (DBP) of 90 mm Hg or more or taking antihypertensive medication.[3] Substantial improvements have been made with regard to enhancing awareness and treatment of hypertension. However, a National Health Examination Survey (NHANES) spanning 2005-2006 showed that 29% of US adults 18 years of age and older were hypertensive; 7% of hypertensive adults had never been told that they had hypertension.
Furthermore, of those with high blood pressure (BP), 78% were aware they were hypertensive, 68% were being treated with antihypertensive agents, and only 64% of treated individuals had controlled hypertension.[3] In addition, data from NHANES 1999-2006 estimated that 30% of adults 20 years of age and older have prehypertension, defined as an untreated SBP of 120-139 mm Hg or untreated DBP of 80-89 mmHg.[3] (See Epidemiology.)
Data from the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7), which was released in 2003, were relatively similar to the NHANES data. The JNC 7 noted that approximately 30% of adults were unaware of their hypertension; up to 40% of people with hypertension were not receiving treatment; and, of those treated, up to 67% did not have their BP controlled to less than 140/90 mm Hg.[4] These data will likely change with the Eighth Report of the JNC (JNC8), which is undergoing editorial review, comment, and approval by The US Department of Health and Human Services (HHS) as of June 2013. (See http://www.nhlbi.nih.gov/guidelines/indevelop.htm#status.)
Hypertension is the most important modifiable risk factor for coronary heart disease (the leading cause of death in North America), stroke (the third leading cause), congestive heart failure, end-stage renal disease, and peripheral vascular disease. Therefore, health care professionals must not only identify and treat patients with hypertension but also promote a healthy lifestyle and preventive strategies to decrease the prevalence of hypertension in the general population. (See Treatment.)
Definition and classificationDefining abnormally high blood pressure (BP) is extremely difficult and arbitrary. Furthermore, the relationship between systemic arterial pressure and morbidity appears to be quantitative rather than qualitative. A level for high BP must be agreed upon in clinical practice for screening patients with hypertension and for instituting diagnostic evaluation and initiating therapy. Because the risk to an individual patient may correlate with the severity of hypertension, a classification system is essential for making decisions about aggressiveness of treatment or therapeutic interventions. (See Presentation.)
Based on recommendations of the JNC 7, the classification of BP (expressed in mm Hg) for adults aged 18 years or older is as follows[4] :
Normal: systolic lower than 120 mm Hg, diastolic lower than 80 mm HgPrehypertension: systolic 120-139 mm Hg, diastolic 80-89 mm HgStage 1: systolic 140-159 mm Hg, diastolic 90-99 mm HgStage 2: systolic 160 mm Hg or greater, diastolic 100 mm Hg or greaterThe classification above is based on the average of 2 or more readings taken at each of 2 or more visits after initial screening.[4, 6] Normal BP with respect to cardiovascular risk is less than 120/80 mm Hg. However, unusually low readings should be evaluated for clinical significance.
Prehypertension, a new category designated in the JNC 7 report, emphasizes that patients with prehypertension are at risk for progression to hypertension and that lifestyle modifications are important preventive strategies.
From another perspective, hypertension may be categorized as either essential or secondary. Primary (essential) hypertension is diagnosed in the absence of an identifiable secondary cause. Approximately 90-95% of adults with hypertension have primary hypertension, whereas secondary hypertension accounts for around 5-10% of the cases.[10] However, secondary forms of hypertension, such as primary hyperaldosteronism, account for 20% of resistant hypertension (hypertension in which BP is >140/90 mm Hg despite the use of medications from 3 or more drug classes, 1 of which is a thiazide diuretic).
Especially severe cases of hypertension, or hypertensive crises, are defined as a BP of more than 180/120 mm Hg and may be further categorized as hypertensive emergencies or urgencies. Hypertensive emergencies are characterized by evidence of impending or progressive target organ dysfunction, whereas hypertensive urgencies are those situations without progressive target organ dysfunction.[4]
In hypertensive emergencies, the BP should be aggressively lowered within minutes to an hour by no more than 25%, and then lowered to 160/100-110 mm Hg within the next 2-6 hours.[4] Acute end-organ damage in the setting of a hypertensive emergency may include the following[11] :
Neurologic: hypertensive encephalopathy, cerebral vascular accident/cerebral infarction, subarachnoid hemorrhage, intracranial hemorrhage Cardiovascular: myocardial ischemia/infarction, acute left ventricular dysfunction, acute pulmonary edema, aortic dissection, unstable angina pectoris Other: acute renal failure/insufficiency, retinopathy, eclampsia, microangiopathic hemolytic anemiaWith the advent of antihypertensives, the incidence of hypertensive emergencies has declined from 7% to approximately 1%.[12] In addition, the 1-year survival rate associated with this condition has increased from only 20% (prior to 1950) to more than 90% with appropriate medical treatment.[13] (See Medication.)
PreviousNextPathophysiologyThe pathogenesis of essential hypertension is multifactorial and highly complex.[14] Multiple factors modulate the blood pressure (BP) for adequate tissue perfusion and include humoral mediators, vascular reactivity, circulating blood volume, vascular caliber, blood viscosity, cardiac output, blood vessel elasticity, and neural stimulation. A possible pathogenesis of essential hypertension has been proposed in which multiple factors, including genetic predisposition, excess dietary salt intake, and adrenergic tone, may interact to produce hypertension. Although genetics appears to contribute to essential hypertension, the exact mechanism has not been established.
Due to investigations into the pathophysiology of hypertension, both in animals and humans, growing evidence suggests that hypertension may have an immunological basis. Studies have revealed that hypertension is associated with renal infiltration of immune cells and that pharmacologic immunosuppression (such as with the drug mycophenolate mofetil) or pathologic immunosuppression (such as occurs with HIV) results in reduced blood pressure in animals and humans. Evidence suggests that T lymphocytes and T-cell derived cytokines (eg, interleukin 17, tumor necrosis factor alpha) play an important role in hypertension. One hypotehesis is that prehypertension results in oxidation and altered mechanical forces that lead to the formation of neoantigens, which are then presented to T cells, leading to T-cell activation and infiltration of critical organs (eg, kidney, vasculature). Thisresultsinpersistentorseverehypertensionandendorgandamage.Sympatheticnervoussystemactivationandnoradrenergicstimulihavealsobeenshownto promote T-lymphocyte activation and infiltration and contribute to the pathophysiology of hypertension.[15, 16, 17]
The natural history of essential hypertension evolves from occasional to established hypertension. After a long invariable asymptomatic period, persistent hypertension develops into complicated hypertension, in which end-organ damage to the aorta and small arteries, heart, kidneys, retina, and central nervous system is evident.
The progression of essential hypertension is as follows:
Prehypertension in persons aged 10-30 years (by increased cardiac output)Early hypertension in persons aged 20-40 years (in which increased peripheral resistance is prominent)Established hypertension in persons aged 30-50 yearsComplicated hypertension in persons aged 40-60 yearsOne mechanism of hypertension has been described as high-output hypertension. High-output hypertension results from decreased peripheral vascular resistance and concomitant cardiac stimulation by adrenergic hyperactivity and altered calcium homeostasis. A second mechanism manifests with normal or reduced cardiac output and elevated systemic vascular resistance due to increased vasoreactivity. Another (and overlapping) mechanism is increased salt and water reabsorption (salt sensitivity) by the kidney, which increases circulating blood volume.
Cortisol reactivity, an index of hypothalamic-pituitary-adrenal function, may be another mechanism by which psychosocial stress is associated with future hypertension.[18] In a prospective substudy of the Whitehall II cohort, with 3 years follow-up of an occupational cohort in previously healthy patients, investigators reported 15.9% of the patient sample developed hypertension in response to laboratory-induced mental stressors and found an association between cortisol stress reactivity and incident hypertension.[18]
PreviousNextEtiologyHypertension may be primary, which may develop as a result of environmental or genetic causes, or secondary, which has multiple etiologies, including renal, vascular, and endocrine causes. Primary or essential hypertension accounts for 90-95% of adult cases, and a small percentage of patients (2-10%) have a secondary cause. Hypertensive emergencies are most often precipitated by inadequate medication or poor compliance.
Environmental and genetic/epigenetic causesHypertension develops secondary to environmental factors, as well as multiple genes, whose inheritance appears to be complex.[13, 19] Furthermore, obesity, diabetes, and heart disease also have genetic components and contribute to hypertension. Epidemiological studies using twin data and data from Framingham Heart Study families reveal that BP has a substantial heritable component, ranging from 33-57%.[20, 21, 22]
In an attempt to elucidate the genetic components of hypertension, multiple genome wide association studies (GWAS) have been conducted, revealing multiple gene loci in known pathways of hypertension as well as some novel genes with no known link to hypertension as of yet.[23] Further research into these novel genes, some of which are immune-related, will likely increase the understanding of hypertension's pathophysiology, allowing for increased risk stratification and individualized treatment.
Epigenetic phenomena, such as DNA methylation and histone modification, have also been implicated in the pathogenesis of hypertension. For example, a high-salt diet appears to unmask nephron development caused by methylation. Maternal water deprivation and protein restriction during pregnancy increase renin-angiotensin expression in the fetus. Mental stress induces a DNA methylase, which enhances autonomic responsiveness. The pattern of serine protease inhibitor gene methylation predicts preeclampsia in pregnant women.[24]
Despite these genetic findings, targeted genetic therapy seems to have little impact on hypertension. In the general population, not only does it appear that individual and joint genetic mutations have very small effects on BP levels, but it has not been shown that any of these genetic abnormalities are responsible for any applicable percentage of cases of hypertension in the general population.[25]
Secondary causes of hypertension related to single genes are very rare. They include Liddle syndrome, glucocorticoid-remediable hyperaldosteronism, 11 beta-hydroxylase and 17 alpha-hydroxylase deficiencies, the syndrome of apparent mineralocorticoid excess, and pseudohypoaldosteronism type II.[4]
Causes of secondary hypertensionRenal causes (2.5-6%) of hypertension include the renal parenchymal diseases and renal vascular diseases, as follows:
Polycystic kidney diseaseChronic kidney diseaseUrinary tract obstructionRenin-producing tumorLiddle syndromeRenovascular hypertension (RVHT) causes 0.2-4% of cases. Since the seminal experiment in 1934 by Goldblatt et al,[26] RVHT has become increasingly recognized as an important cause of clinically atypical hypertension and chronic kidney disease—the latter by virtue of renal ischemia. The coexistence of renal arterial vascular (ie, renovascular) disease and hypertension roughly defines this type of nonessential hypertension. More specific diagnoses are made retrospectively when hypertension is improved after intravascular intervention.
Vascular causes include the following:
Coarctation of aortaVasculitisCollagen vascular diseaseEndocrine causes account for 1-2% and include exogenous or endogenous hormonal imbalances. Exogenous causes include administration of steroids. The most common form of secondary hypertension is a renal cause (although the true prevalence of hyperaldosteronism is not clear).
Another common cause is endocrine: oral contraceptive use. Activation of the renin-angiotensin-aldosterone system (RAAS) is the likely mechanism, because hepatic synthesis of angiotensinogen is induced by the estrogen component of oral contraceptives. Approximately 5% of women taking oral contraceptives may develop hypertension, which abates within 6 months after discontinuation. The risk factors for oral contraceptive–associated hypertension include mild renal disease, familial history of essential hypertension, age older than 35 years, and obesity. It would be better to group oral contraceptives and steroids with drug-induced hypertension (see Table 1, below).
Exogenous administration of the other steroids used for therapeutic purposes also increases blood pressure (BP), especially in susceptible individuals, mainly by volume expansion. Nonsteroidal anti-inflammatory drugs (NSAIDs) may also have adverse effects on BP. NSAIDs block both cyclooxygenase-1 (COX-1) and COX-2 enzymes. The inhibition of COX-2 can inhibit its natriuretic effect, which, in turn, increases sodium retention. NSAIDs also inhibit the vasodilating effects of prostaglandins and the production of vasoconstricting factors—namely, endothelin-1. These effects can contribute to the induction of hypertension in a normotensive or controlled hypertensive patient.
Endogenous hormonal causes include the following:
Primary hyperaldosteronismCushing syndromePheochromocytomaCongenital adrenal hyperplasiaNeurogenic causes include the following:
Brain tumorBulbar poliomyelitisIntracranial hypertensionDrugs and toxins that cause hypertension include the following:
AlcoholCocaineCyclosporine, tacrolimusNSAIDsErythropoietinAdrenergic medicationsDecongestants containing ephedrineHerbal remedies containing licorice (including licorice root) or ephedrine (and ephedra)NicotineOther causes include the following:
Hyperthyroidism and hypothyroidismHypercalcemiaHyperparathyroidismAcromegalyObstructive sleep apneaPregnancy-induced hypertensionObstructive sleep apnea (OSA) is a common but frequently undiagnosed sleep-related breathing disorder defined as an average of at least 10 apneic and hypopenic episodes per sleep hour, which leads to excessive daytime sleepiness. Multiple studies have shown OSA to be an independent risk factor for the development of essential hypertension, even after adjusting for age, gender, and degree of obesity.
Approximately half of individuals with hypertension have OSA, and approximately half with OSA have hypertension. Ambulatory BP monitoring normally reveals a "dip" in BP of at least 10% during sleep. However, if a patient is a "nondipper," the chances that the patient has OSA is increased. Nondipping is thought to be caused by frequent apneic/hypopneic episodes that end with arousals associated with marked spikes in BP that last for several seconds.
Numerous studies have shown that treatment of OSA by continuous positive airway pressure (CPAP) or position therapy lowers the awake and 24-hour blood pressure levels. Unfortunately, most cases of OSA go undiagnosed. Improved physician awareness and screening for this reversible cause of hypertension is likely to lead to great improvements in quality of life and a reduced incidence of cardiovascular complications.[27]
Causes of hypertensive emergenciesThe most common hypertensive emergency is a rapid unexplained rise in BP in a patient with chronic essential hypertension. Most patients who develop hypertensive emergencies have a history of inadequate hypertensive treatment or an abrupt discontinuation of their medications.[28, 29]
Other causes of hypertensive emergencies include the use of recreational drugs, abrupt clonidine withdrawal, post pheochromocytoma removal, and systemic sclerosis, as well as the following:
Renal parenchymal disease: chronic pyelonephritis, primary glomerulonephritis, tubulointerstitial nephritis (accounts for 80% of all secondary causes) Systemic disorders with renal involvement: systemic lupus erythematosus, systemic sclerosis, vasculitidesRenovascular disease: atherosclerotic disease, fibromuscular dysplasia, polyarteritis nodosaEndocrine disease: pheochromocytoma, Cushing syndrome, primary hyperaldosteronismDrugs: cocaine,[30] amphetamines, cyclosporine, clonidine (withdrawal), phencyclidine, diet pills, oral contraceptive pills Drug interactions: monoamine oxidase inhibitors with tricyclic antidepressants, antihistamines, or tyramine-containing foodCentral nervous system factors: CNS trauma or spinal cord disorders, such as Guillain-Barré syndromeCoarctation of the aortaPreeclampsia/eclampsiaPostoperative hypertensionPreviousNextEpidemiologyHypertension is a worldwide epidemic; accordingly, its epidemiology has been well studied. Data from National Health and Nutrition Examination Survey (NHANES) spanning 1999-2002 in the United States found that in the population aged 20 years or older, an estimated 41.9 million men and 27.8 million women had prehypertension, 12.8 million men and 12.2 million women had stage 1 hypertension, and 4.1 million men and 6.9 million women had stage 2 hypertension.[31] Data from NHANES spanning 2003–2006 showed that 33.6% of US adults 20 years of age have hypertension, resulting in an estimated 74.5 million US adults with hypertension.
In many countries, 50% of the population older than 60 years have hypertension. Overall, approximately 20% of the world’s adults are estimated to have hypertension. The 20% prevalence is for hypertension defined as blood pressure (BP) in excess of 140/90 mm Hg. The prevalence dramatically increases in patients older than 60 years.
In a large Spanish epidemiologic study over a 10-year period, investigators found that despite an increase in the intensity of hypertensive therapy, the prevalence of uncontrolled hypertension (systolic BP [SBP] ≤140 mm Hg and/or diastolic BP [DBP] ≤90 mm Hg) did not change significantly over time.[32] In addition, there appeared to be worse control in at-risk individuals (SBP ≤130 mm Hg and/or DBP ≤80-85 mm Hg) who had comorbidities.
Hypertension and sex- and age-related statisticsUntil age 45 years, a higher percentage of men than women have hypertension; from age 45 years onward, the percentages are nearly equal between men and women. In women, those who use oral contraceptives, particularly obese and older women, have a 2- to 3-fold higher risk of hypertension than women not using these agents.
Hypertension in black adultsGlobally, black adults have among the highest rates of hypertension, with an increasing prevalence. Although white adults also have an increasing incidence of high BP, they develop this condition later in life than black adults and have much lower average BPs. In fact, compared to hypertensive white persons, hypertensive black individuals have a 1.3-fold higher rate of nonfatal stroke, a 1.8-fold higher rate of fatal stroke, a 1.5-fold higher mortality rate due to heart disease, and a 4.2-fold higher rate of end-stage renal disease (ESRD).
Table 1, below, summarizes age-adjusted prevalence estimates from the National Health Interview Survey (NHIS) and the National Center for Health Statistics (NCHS) according to racial/ethnic groups and diagnosed conditions in individuals 18 years of age and older.[33, 34]
Table 1. NHIS/NCHS Age-Adjusted Prevalence Estimates in Individuals Aged 18 Years and Older in 2008. (Open Table in a new window)
Race/Ethnic Group Have Hypertension, % Have Heart Disease, % Have Coronary Heart Disease, % Have Had a Stroke, % White only23.312.16.52.7Black/African American31.810.25.63.6Hispanic/Latino21.08.15.72.6Asian21.05.22.91.8American Indian/Alaska Native25.312.16.6 (this number is considered unreliable)3.9 (this number is considered unreliable)Source:Â Pleis JR, Lucus JW, Ward BW. Summary health statistics for US adults: National Health Interview Survey, 2008. Vital Health Stat 10. No. 242; 2009. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_242.pdf. Accessed: February 21, 2012.NCHS = National Center for Health Statistics; NHIS = National Health Interview Survey.
PreviousNextPrognosis
Most individuals diagnosed with hypertension will have increasing blood pressure (BP) as they age. Untreated hypertension is notorious for increasing the risk of mortality and is often described as a silent killer. Mild to moderate hypertension, if left untreated, may be associated with a risk of atherosclerotic disease in 30% of people and organ damage in 50% of people within 8-10 years after onset.
Death from ischemic heart disease or stroke increases progressively as BP increases. For every 20 mm Hg systolic or 10 mm Hg diastolic increase in BP above 115/75 mm Hg, the mortality rate for both ischemic heart disease and stroke doubles.[4]
Hypertensive retinopathy was associated with an increased long-term risk of stroke, even in patients with well-controlled BP, in a report of 2907 adults with hypertension participating in the Atherosclerosis Risk in Communities (ARIC) study.[35, 36] Increasing severity of hypertensive retinopathy was associated with an increased risk of stroke; the stroke risk was 1.35 in the mild retinopathy group and 2.37 in the moderate/severe group.
The morbidity and mortality of hypertensive emergencies depend on the extent of end-organ dysfunction on presentation and the degree to which BP is controlled subsequently. With BP control and medication compliance, the 10-year survival rate of patients with hypertensive crises approaches 70%.[37]
In the Framingham Heart Study, the age-adjusted risk of congestive heart failure was 2.3 times higher in men and 3 times higher in women when the highest BP was compared to the lowest BP.[38] Multiple Risk Factor Intervention Trial (MRFIT) data showed that the relative risk for coronary artery disease mortality was 2.3 to 6.9 times higher for persons with mild to severe hypertension than it was for persons with normal BP.[39] The relative risk for stroke ranged from 3.6 to 19.2. The population-attributable risk percentage for coronary artery disease varied from 2.3 to 25.6%, whereas the population-attributable risk for stroke ranged from 6.8-40%.
The Framingham Heart Study found a 72% increase in the risk of all-cause death and a 57% increase in the risk of any cardiovascular event in patients with hypertension who were also diagnosed with diabetes mellitus.[40]
Nephrosclerosis is one of the possible complications of long-standing hypertension. The risk of hypertension-induced end-stage renal disease is higher in black patients, even when blood pressure is under good control. Furthermore, patients with diabetic nephropathy who are hypertensive are also at high risk for developing end-stage renal disease.
Comparative data from the NHANES I and III showed a decrease in mortality over time in hypertensive adults, but the mortality gap between hypertensive and normotensive adults remained high.[41]
Clinical trials have demonstrated the following benefits with antihypertensive therapy[4] :
Average 35-40% reduction in stroke incidenceAverage 20-25% reduction in myocardial infarctionAverage >50% reduction in heart failureMoreover, it is estimated that 1 death is prevented per 11 patients treated for stage 1 hypertension and other cardiovascular risk factors when a sustained reduction of 12 mm Hg in systolic BP over 10 years is achieved.[4] However, for the same reduction is systolic BP reduction, it is estimated that 1 death is prevented per 9 patients treated when cardiovascular disease or end-organ damage is present.[4]
PreviousNextPatient EducationHypertension is a lifelong disorder. For optimal control, a long-term commitment to lifestyle modifications and pharmacologic therapy is required. Therefore, repeated in-depth patient education and counseling not only improve compliance with medical therapy but also reduce cardiovascular risk factors.
Various strategies to decrease cardiovascular disease risk include the following:
Prevention and treatment of obesity: an increase in body mass index (BMI) and waist circumference is associated with an increased risk of developing conditions with high cardiovascular risk, such as hypertension, diabetes mellitus, impaired fasting glucose, and left ventricular hypertrophy [LVH][42] Appropriate amounts of aerobic physical activityDiets low in salt, total fat, and cholesterolAdequate dietary intake of potassium, calcium, and magnesiumLimited alcohol consumptionAvoidance of cigarette smokingAvoidance of the use of illicit drugs, such as cocainePreviousProceed to Clinical Presentation , Hypertension





0 comments:
Post a Comment