Cardiac rhythms arising from the atrioventricular (AV) junction occur as an automatic tachycardia or as an escape mechanism during periods of significant bradycardia with rates slower than the intrinsic junctional pacemaker.
The AV node (AVN) has intrinsic automaticity that allows it to initiate and depolarize the myocardium during periods of significant sinus bradycardia or complete heart block. This escape mechanism, with a rate of 40-60 beats per minute, produces a narrow QRS complex because the ventricle is depolarized using the normal conduction pathway. An accelerated junctional rhythm (rate >60) is a narrow complex rhythm that often supersedes a clinically bradycardic sinus node rate (see images below). The QRS complexes are uniform in shape, and evidence of retrograde P wave activation may or may not be present.
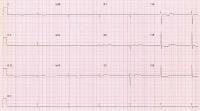 Junctional bradycardia due to profound sinus node dysfunction. No atrial activity is apparent.
Junctional bradycardia due to profound sinus node dysfunction. No atrial activity is apparent.  Note the retrograde P waves that precede each QRS complex.
Note the retrograde P waves that precede each QRS complex. Less commonly, the AV junction develops abnormal automaticity and exceeds the sinus node rate at a time when the sinus rate would be normal (see image below). These junctional tachycardias are most often observed in the setting of digitalis toxicity, recent cardiac surgery, acute myocardial infarction, or isoproterenol infusion.
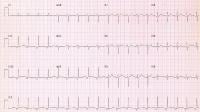 Accelerated junctional rhythm is present in this patient. Note the inverted P waves that precede each QRS complex, with a rate of 115 bpm. NextPathophysiology
Accelerated junctional rhythm is present in this patient. Note the inverted P waves that precede each QRS complex, with a rate of 115 bpm. NextPathophysiologyThe junctional rhythm initiates within the AV nodal tissue. Accelerated junctional rhythm is a result of enhanced automaticity of the AVN that supersedes the sinus node rate. During this rhythm, the AVN is firing faster than the sinus node, resulting in a regular narrow complex rhythm. These rhythms may demonstrate retrograde P waves on ECG findings, and the rates can vary from 40-60 beats per minute.
Changes in autonomic tone or the presence of sinus node disease that is causing an inappropriate slowing of the sinus node may exacerbate this rhythm. Young healthy individuals, especially those with increased vagal tone during sleep, are often noted to have periods of junctional rhythm that is completely benign, not requiring any intervention.
Rarely, the AVN develops enhanced automaticity and overtakes a "normal" sinus node. This occasionally is observed in digitalis toxicity, following cardiac surgery (typically valve replacement), during acute myocardial infarction, or during isoproterenol infusion. Alteration in calcium metabolism in the sarcoplasmic reticulum causes accelerated junctional rhythm.[1]
PreviousNextEpidemiologyFrequencyUnited StatesJunctional rhythms are common in patients with sick sinus syndrome or in patients who have significant bradycardia that allows the AV nodal region to determine the heart rate.
Mortality/MorbidityThe heart rate during a junctional rhythm often determines whether the patient has symptoms.Presence of AV disassociation can lead to symptoms in patients because of atrial conduction and subsequent contraction when the tricuspid valve is closed (ie, canon a waves). Periods of junctional rhythm are not necessarily associated with an increase in mortality. If an obvious cause is present, such as complete heart block or sick sinus syndrome, then the morbidity or mortality is directly related to that and not to the junctional rhythm mechanism, which is serving as a "backup rhythm" during the periods of bradycardia. Accelerated junctional rhythms may be a sign of digitalis toxicity. SexJunctional escape rhythms, which are common in younger and/or athletic individuals during periods of increased vagal tone (eg, sleep), occur equally in males and females.
AgeThis rhythm may occur in persons of any age.Junctional rhythms during sleep are common in children and in athletic adults.PreviousProceed to Clinical Presentation , Junctional Rhythm





0 comments:
Post a Comment