Despite recent declines in age-adjusted mortality, in 2005, cardiovascular disease (CVD) was the primary cause in 864,480 deaths (35.3% of total) and the secondary cause in another 507,520 deaths in the United States.[1] In fact, CVD has been the leading cause of death in the United States for the past 100 years, except for 1918.[1] While CVD age-adjusted death rates are reportedly declining in the United States, they are increasing in many developing countries. These developing countries and emerging market economies are succumbing to the epidemiologic transition that afflicted the United States (CVD-related mortality), posing a major challenge to these regions as they undergo social and economic development as emerging market economies.[2, 3, 4]
The most preventable form of CVD is coronary heart disease (CHD). In the United States, CHD annually results in 502,000 deaths, of which 185,000 are due to myocardial infarction (MI); 1.2 million MIs, of which 700,000 are first infarctions; and an economic burden of $133 billion.
An American Health Association policy statement concluded that costs will rise to more than $1 trillion annually in the United States by the year 2030, thus suggesting the great need for preventative measures.[5]
Currently, 16.8 million Americans (8.7 million men, 8.1 million women) have documented CHD.[4] Asymptomatic disease is even more prevalent. By the year 2020, CHD is estimated to become the leading cause of death and disability worldwide. Despite this high prevalence, evidence increasingly suggests that the atherosclerotic process can be greatly slowed and its consequences markedly reduced by preventive measures. Primordial prevention usually refers to healthy lifestyle choices to prevent the development of coronary risk factors.[6] Primary prevention deals with delaying or preventing the onset of cardiovascular disease (MeSH definition).
Many countries where CHD is on the rise have instituted counselling and educational methods to encourage people to reduce their risks for developing heart disease. A review examined 55 trials intended to reduce multiple risk factors; the trials lasted between 6 months and 12 years and were conducted in several countries over the course of 4 decades. The review suggested that intervention results in small reductions in risk factors, including blood pressure, cholesterol, and smoking, but has little or no impact on the risk of CHD mortality or morbidity.[7] This demonstrates that a different approach to behavior change is needed, particularly in developing countries where cardiovascular disease rates are rising.
A study by Pande et al suggests millions of US adults with peripheral arterial disease (PAD) are not receiving secondary prevention therapies.[8] PAD was defined as an ankle-brachial index of 0.90 or less. Of 7458 eligible participants aged 40 years or older, weighted PAD prevalence was 5.9±0.3%, corresponding to approximately 7.1 million US adults with PAD. Treatment with multiple therapies (statins, ACE inhibitor/angiotensin receptor blockers, and aspirin) is associated with reduced all-cause mortality.
Secondary prevention relies on early detection of disease process and application of interventions to prevent progression of disease (MeSH definition). This article summarizes the guidelines for the primary and secondary prevention of CHD.
NextRisk Assessment and Primary PreventionRisk Factors and Risk ScoresPrimary prevention reduces MI and heart failure, decreases the need for coronary revascularization procedures, and extends and improves the quality of life. The American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, in a 2010 report on cardiovascular risk assessment in asymptomatic adults, recommends obtaining global risk scores (eg, Framingham Risk Score[9] ) and a family history of cardiovascular disease for cardiovascular risk assessment.[10]
The Framingham Heart Study first introduced the term risk factor into modern medical literature; the term is generally applied to a parameter that is predictive of a future cardiovascular event. Broadly, risk factors are arbitrarily divided into 3 major categories:
Table 1. Basic Categories of Risk Factors for Future Cardiovascular Event (Open Table in a new window)
Category Risk Factors Nonmodifiable risk factorsAge, sex, family history, geneticModifiable risk factorsSmoking, atherogenic diet, alcohol intake, physical activity, dyslipidemias, hypertension, obesity, diabetes, metabolic syndromeEmerging risk factorsC-reactive protein (CRP), fibrinogen, coronary artery calcification (CAC), homocysteine, lipoprotein(a), and small, dense LDLAdapted from ATP III Final Report 2002, ATP III Update 2004: Implications of Recent Clinical Trials for the ATP III Guidelines[11]
Several risk scores have been developed to help predict an individual's risk of future cardiovascular events. For example, the Framingham Heart Study developed a coronary risk estimate using some of the following major traditional risk factors:
AgeGenderFamily history of premature CHD (first-degree male relative Elevated total or LDL cholesterol levelReduced HDL cholesterol levelSmokingHypertensionDiabetes mellitusObesitySedentary lifestyleUsing these risk factors, a Framingham score can be computed that helps assess the 10-year risk of CHD for individuals with risk factors. The American Heart Association suggests childhood obesity is likely to lower the age of onset and increase the incidence of cardiovascular disease worldwide.[12]
Berry et al suggest that differences in risk-factor burden result in marked differences in the lifetime risk for cardiovascular disease. They also conclude that these differences are consistently noted across both race and birth cohorts.[13]
The following tables are adapted from NHLBI Web site.[9] Note that diabetes is excluded because it constitutes coronary artery disease risk equivalent.
NCEP/Framingham Estimate of 10-Year Coronary Heart Disease Risk in MenTable 2. Framingham Point Scores by Age Group in Men (Open Table in a new window)
AgePoints20-34-935-39-440-44045-49350-54655-59860-641065-691170-741275-7913Table 3. Framingham Point Scores by Age Group and Total Cholesterol in Men (Open Table in a new window)
Total CholesterolAge 20-39Age 40-49Age 50-59Age 60-69Age 70-7900000160-19943210200-23975310240-27996421280+118531Table 4. Framingham Point Scores by Age and Smoking Status in Men (Open Table in a new window)
Age 20-39Age 40-49Age 50-59Age 60-69Age 70-79Nonsmoker00000Smoker85311Table 5. Framingham Point Scores by HDL level in Men (Open Table in a new window)
HDLPoints60+-150-59040-4912Table 6. Framingham Point Scores by Systolic Blood Pressure and Treatment Status in Men (Open Table in a new window)
Systolic BPIf UntreatedIf Treated00120-12901130-13912140-15912160+23Table 7. 10-Year Risk by Total Framingham Point Scores in Men (Open Table in a new window)
Point Total10-Year Risk01%11%21%31%41%52%62%73%84%95%106%118%1210%1312%1416%1520%1625%17 or more≥30%NCEP/Framingham Estimate of 10-Year Coronary Heart Disease Risk in WomenTable 8. Framingham Point Scores by Age Group in Women (Open Table in a new window)
AgePoints20-34-735-39-340-44045-49350-54655-59860-641065-691270-741475-7916Table 9. Framingham Point Scores by Age Group and Total Cholesterol in Women (Open Table in a new window)
Total CholesterolAge 20-39Age 40-49Age 50-59Age 60-69Age 70-7900000160-19943211200-23986421240-279118532280+1310742Table 10. Framingham Point Scores by Age and Smoking Status in Women (Open Table in a new window)
Age 20-39Age 40-49Age 50-59Age 60-69Age 70-79Nonsmoker00000Smoker97421Table 11. Framingham Point Scores by HDL level in Women (Open Table in a new window)
HDLPoints60+-150-59040-4912Table 12. Framingham Point Scores by Systolic Blood Pressure and Treatment Status in Women (Open Table in a new window)
Systolic BPIf UntreatedIf Treated00120-12913130-13924140-15935160+46Table 13. 10-Year Risk by Total Framingham Point Scores in Women (Open Table in a new window)
Point Total10-Year Risk91%101%111%121%132%142%153%164%175%186%198%2011%2114%2217%2322%2427%25 or more≥30%Prevalence of coronary risk factors in the United States are as follows:
LDL cholesterol >130 mg/dL – 46%HDL cholesterol 40 mg/dL – 26%Prehypertension – 22%Hypertension – 25%Tobacco use – 25%Diabetes mellitus – 8%Overweight or obese – 65%Physically inactive – 38%Metabolic syndrome – 24%Considerable clinical benefit can be derived from the management of 3 major modifiable coronary risk factors: hypercholesterolemia, hypertension, and cigarette smoking.
According to the Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research (EISNER), the addition of CAC scanning to conventional risk factor modification has been associated with superior coronary artery disease risk factor control without increasing downstream medical testing.[14]
Every 1 mmol/L (38.7 mg/dL) decline in LDL cholesterol results in a 21% decrease in cardiovascular events.[15] A decrease in systolic blood pressure by 10 mm Hg can decrease cardiovascular mortality by 20-40%.[16, 17, 18] Similarly, the risk of acute MI increases by 5.6% for every additional cigarette smoked per day.[19]
Hypercholesterolemia/dyslipidemiaScreening should include a full fasting lipid profile including total cholesterol, HDL, and triglycerides measurements. The ratio of total or LDL cholesterol to HDL appears to be a powerful risk predictor.[20] The Adult Treatment Panel III NCEP guidelines, published in 2001, include initiation of lifestyle and drug management with the following goals.
A primary goal of reducing LDL cholesterol level is as follows:
20% 10-year Framingham riskSecondary goals are as follows:
If LDL goals are achieved and triglyceride levels are >200 mg/dL, the goal for non-HDL cholesterol level should be set at 30 mg/dL higher than the LDL cholesterol level. In response to the recent trial results, the NCEP has recommended lowering of the LDL target goals to [21] The value of intensive cholesterol reduction is best documented for patients with CHD in the recent IVUS, ASTEROID, and PROVE-IT trials, studying atherosclerosis progression and coronary events, respectively. Their statement acknowledges that the recent trials have failed to demonstrate an LDL cholesterol level below which coronary risk does not decrease. Measurement of HDL cholesterol should be used as part of the initial cardiovascular risk assessment but should not be used as a predictive tool of residual vascular risk in patients who are treated with potent high-dose statin therapy to lower LDL cholesterol.[22] The extended follow-up of the Heart Protection Study (HPS) assessed the long-term efficacy and safety of lowering LDL cholesterol with statins, and found that prolonged LDL-lowering statin treatment produces larger absolute reductions in vascular events. The benefits of long-term continuation of statin treatment persisted for at least 5 years without any evidence of developing risks.[23] On the basis of the JUPITER trial, European health authorities have suggested that when LDL cholesterol levels do not require pharmacologic treatment, 20 mg of rosuvastatin significantly reduces major cardiovascular events in primary prevention patients with elevated high-sensitivity C-reactive protein who have high global cardiovascular risk (10-year Framingham risk score >20%).[24] The Multi-Ethnic Study of Atherosclerosis (MESA) studied eligible participants from the JUPITER trial to assess whether or not coronary artery calcium (CAC) might further stratify risk. The results suggest that in the patients eligible for JUPITER, CAC could be used to target subgroups of patients who are expected to derive the most, and the least, absolute benefit from statin treatment.[25] Secondary causes of dyslipidemiaBefore therapy is initiated, the following potential secondary causes of dyslipidemia should be considered based on the associated dyslipidemia:
High LDL: Hypothyroidism[26, 27] , nephrotic syndrome, primary biliary cirrhosis[28] , and anorexia nervosa[29, 30] Hypertriglyceridemia: Diabetes mellitus[31] , chronic kidney disease, alcoholism, pregnancy[32] , hypothyroidism[26, 27] Low HDL: Diabetes mellitus, cigarette smoking[33, 34] , obesity[35]Table 14. Proposed Modifications of ATP III LDL-Cholesterol Goals and Cut Points for Therapeutic Lifestyle Changes and Drug Therapy in Different Risk Categories[36] (Open Table in a new window)
Risk CategoryLDL GoalLDL level at which to Initiate Therapeutic Lifestyle ChangesLDL level at which to Consider DrugTherapy§
High risk - CHD or CHD risk equivalent (10-y risk >20%)***≥100 mg/dL║≥100 mg/dL,¶Moderate-high risk - 2 or more risk factors (10-y risk 10-20%)†††≥130 mg/dL≥130 mg/dL; 100-129mg/dL consider drug options#Moderate risk - 2 or more risk factors (10-year risk ≥130 mg/dL≥160 mg/dLLower risk - 0-1 risk factor‡≥160 mg/dL≥190 mg/dL; 160-189 mg/dL consider drug options* Heart disease risk equivalents include noncoronary forms of atherosclerotic disease (peripheral arterial disease, abdominal aortic aneurysm, and carotid artery disease) and diabetes. Ten-year risk defined by modified Framingham risk score.
†Risk factors that modify LDL goals include cigarette smoking; hypertension (BP ≥140/90 mm Hg or on antihypertensive medications); low HDL cholesterol (
‡ Almost all people with 0-1 risk factor have a 10-year risk of less than 10%; thus, 10-year risk assessment in people with 0-1 risk factor is not necessary.
§ When LDL-lowering drug therapy is given, the intensity of therapy should be sufficient to achieve at least a 30-40% reduction in LDL levels.
â•‘ Any individual at high or moderately high risk who has lifestyle-related risk factors (eg, obesity, physical inactivity, hypertriglyceridemia, low HDL cholesterol [
¶ If baseline LDL is
# For moderately high-risk persons with LDL of 100-129 mg/dL at baseline or after lifestyle changes, initiation of an LDL-lowering drug to achieve an LDL of less than 100 mg/dL is an option.
** Very high risk favors the optional LDL goal of
††Optional LDL goal of
Triglycerides
Data on the impact of triglycerides on CHD events is not as clearly evident. However, meta-analyses data suggest that elevated triglyceride levels are an independent risk factor for CHD[37, 38] , and data on the benefits of reducing triglyceride levels were demonstrated by using the drug gemfibrozil (fibric acid derivative) in a population with low HDL level ([39, 40]
Non-HDL cholesterolIn patients with mixed dyslipidemia (elevated LDL cholesterol and triglyceride levels), non-HDL cholesterol is a useful measurement. Non-HDL cholesterol represents very LDL cholesterol plus LDL cholesterol, both of which are apo B-100–containing atherogenic lipoprotein fractions. In hypertriglyceridemic individuals, non-HDL cholesterol goals are 30 mg/dL higher than the corresponding LDL goals, representing a triglyceride goal of 150 mg/dL. Non-HDL cholesterol can be measured in a nonfasting state. Non-HDL cholesterol was found to be more predictive of future CV events than LDL in several trials, probably because it measures both of the atherogenic apo B–containing fractions.[41, 42] LDL and total cholesterol/HDL cholesterol ratios are also strongly predictive of CVD risk.[20]
Secondary preventionWhen drug therapy is indicated for reducing LDL cholesterol, statins are generally initiated as first-line therapy. Exceptions include pregnancy, hepatic disease, or history of myositis while on these agents. Resins, nicotinic acid, or ezetimibe can be added if LDL cholesterol level is not reduced to goal. Pharmacologic therapy for triglyceridemia includes fibrates, nicotinic acid, and omega-3 fatty acids. Fibrates and nicotinic acid are also effective in raising low HDL, particularly when high triglycerides are present.
In mixed dyslipidemias, a statin may be combined with nicotinic acid or a fibrate. As described earlier, non-HDL cholesterol is a useful parameter to monitor therapy results in mixed dyslipidemia. When using combined therapy, particularly statins plus fibrates, the risk of myositis increases and, therefore, patients should be educated about muscle symptoms. To minimize the risk of statin myopathy, the statin dose should be kept as low as possible to achieve the LDL goal, and it may be helpful to separate the dosing of statins and fibrates to evening and morning, respectively.
Varespladib methyl 500 mg once daily may be an effective antiatherosclerotic agent.[43]
Compared with placebo or statin monotherapy, evacetrapib as monotherapy or in combination with statins increased HDL-C levels and decreased LDL-C levels. However, further investigation is warranted.[44]
Blood Pressure ControlHypertension is a well-established risk factor for adverse cardiovascular outcomes, including CHD. Systolic blood pressure is at least as powerful a coronary risk factor as the diastolic blood pressure. Isolated systolic hypertension is now established as a major hazard for CHD. Compelling data from meta-analyses indicate that a reduction of diastolic blood pressure by 5-6 mm Hg results in a reduction of stroke risk by 42% and CHD events by 15%.[45]
The self-management of hypertension, which includes self-monitoring of blood pressure and self-titration of antihypertensive drugs, along with telemonitoring of home blood pressure measurements, is an important new addition to the control of hypertension in primary care. Patients who self-manage hypertension have experienced a decrease in systolic blood pressure compared to those who sought usual care.[46] The Clinical Evaluation of Remote Notification to Reduce Time to Clinical Decision (CONNECT) trial found that wireless remote monitoring with automatic clinician alerts significantly reduced the time to a clinical decision in response to clinical events as well as reduced the length of hospital stay.[47]
In patients with mild hypertension (systolic 140-159 mm Hg or diastolic 90-99 mm Hg), the following is noted:
Despite side effects and cost of antihypertensive medications, the beneficial effects of treatment may outweigh the risks, even in low-risk patients. Treatment, if necessary, is initiated with a low-dose of a once-a-day antihypertensive drug in an attempt to minimize future cardiovascular risk after a prolonged trial of nonpharmacologic therapy. One such antihypertensive medication that is used worldwide is hydrochlorothiazide (HCTZ). A daily dose of 12.5-25 mg was measured in head-to-head studies using ambulatory blood pressure measurement and was shown to be consistently inferior to all other drug classes. Because data is lacking for dosing, HCTZ is an inappropriate first-line drug for the treatment of hypertension.[48]In individuals with high-normal blood pressure (systolic 130-139 mm Hg and/or diastolic 85-89 mm Hg), the following is noted:
These persons have an increased risk of cardiovascular events over time compared with those who have optimal blood pressure.Antihypertensive drug therapy should be considered among such patients if diabetes or end-organ damage is present.Treatment, particularly with an angiotensin-converting enzyme (ACE) inhibitor or, if not tolerated, an angiotensin-II receptor blocker, is also warranted in patients with renal insufficiency, diabetes mellitus, or heart failure to slow the progression of the underlying disease. DietTwo types of dietary guidelines exist.
The first type recommends specific quantities of macronutrients, such as [49, 50]
A second type recommends the consumption and exclusion of specific foods, often in combination. An example is the recommendation to eat the following foods to lower cholesterol: stanol/sterol ester margarines, soy products, soluble fiber, and almonds or walnuts. This specific food portfolio recommendation has been found to lower LDL cholesterol more than an AHA Step 2 approach (29% vs 8%, respectively). The reductions were, in fact, equivalent to those of lovastatin 20 mg.[51] Total allowed daily fat ranges from 25-35% of total daily calories provided that saturated fats and trans-fatty acids are kept low.
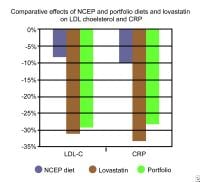 A diet containing stanol-enriched margarine, soy products, high-fiber foods, and almonds reduced LDL cholesterol and CRP more than an NCEP diet. The reductions were equivalent to lovastatin 20 mg.
A diet containing stanol-enriched margarine, soy products, high-fiber foods, and almonds reduced LDL cholesterol and CRP more than an NCEP diet. The reductions were equivalent to lovastatin 20 mg. The Third ATP of the NCEP further modified its dietary recommendations to include a more intense and effective eating plan than previously advocated. Specific recommendations are as follows: 1) Saturated fat,
In general, diets containing unsaturated fats, whole grains, fruits, vegetables, fish, and moderate alcohol are optimal for preventing heart disease.[52] The revised AHA guidelines place emphasis on foods and an overall eating pattern, rather than on percentages of food components such as fat.
One meta-analysis studied the effect of a Mediterranean diet on metabolic syndrome.[53] The diet is characterized by high consumption of monounsaturated fatty acids, primarily from olives and olive oil, and encourages daily consumption of fruits, vegetables, whole grain cereals, and low-fat dairy products; weekly consumption of fish, poultry, tree nuts, and legumes; a relatively low consumption of red meat, approximately twice a month; as well as a moderate daily consumption of alcohol, normally with meals. Adherence to the diet was associated with reduced risk of metabolic syndrome and reduced HDL-cholesterol levels and triglycerides levels. The results are of considerable public health importance because this dietary pattern can be easily adopted by all population groups and various cultures and is cost-effective.
A separate meta-analysis performed by Nordmann et al found that the Mediterranean diet had more favorable changes in weighted mean differences of body weight, body mass index, systolic blood pressure, diastolic blood pressure, fasting plasma glucose, total cholesterol, and high-sensitivity C-reactive protein than low-fat diets.[54]
Of note, in a recently published prospective study, dietary supplementation with marine n−3 fatty acids (eicosapentaenoic acid [EPA], docosahexaenoic acid [DHA] and the plant-derived alpha-linolenic acid [ALA]) did not significantly reduce the rate of cardiovascular events among patients with a prior myocardial infarction.[55]
AlcoholModerate alcohol consumption (1-2 drinks per d) is associated with a reduced overall and CHD-related mortality compared with both abstinence and heavy drinking.[56, 57]
Alcohol raises HDL (by stimulating the hepatic production of apo A-I and A-II)[58, 59, 60] , stimulates fibrinolysis[61, 62, 63] , reduces fibrinogen levels[64, 65] , reduces inflammation[66] , and inhibits platelet activation[67] .
In the United States, additional antioxidant effects have been attributed to red wine, but the consumption of other alcoholic beverages is associated with a somewhat lower or similar reduction in CHD risk[68, 69] , and the pattern and amount of alcohol intake appears to be more important than the type.
AntioxidantsAlthough several observational studies and 1 randomized, controlled secondary prevention trial (CHAOS)[70] found reduced CVD in those taking large amounts of antioxidant vitamins, the HOPE[71] GISSI-Prevention[72] , and Heart Protection Studies (HPS) found no benefit for 400 and 300 IU/d of vitamin E, respectively.[11]
A current meta-analysis of available data suggests no benefit for antioxidant vitamins.[73]
HerbalsAn estimated 40% of Americans use herbal remedies, and at least $15 billion is spent annually in North America on alternative forms of health care. Inquiry about the use of herbals is a component of good medical care, especially in cardiovascular medicine.
Alternative medicine approaches to cholesterol lowering include garlic, policosanol, gugulipid, and red rice yeast extracts, the latter of which contains HMG-CoA reductase inhibitors. Garlic modestly lowers cholesterol (approximately 3%) and may lower BP and inhibit platelet aggregation. Fermented red rice yeast extracts contain statins and lower cholesterol 13-26%.[74] Ephedra-containing herbals, often used as anorexics, are associated with hypertension and stroke and have been banned in the United States.[75, 76]
Summary of General Nutritional RecommendationsAchieve and maintain ideal body weight by limiting foods high in calories and low in nutrition, including those high in sugar, such as soft drinks and candy.
Eat a variety of fruits; vegetables; legumes; nuts; soy products; low-fat dairy products; and whole grain breads, cereals, and pastas.
Eat baked or broiled fish at least twice per week.
Choose oils and margarines low in saturated fat and high in omega-3 fat, such as canola, soybean, walnut, and flaxseed oils, including those fortified with stanols and sterols.
Avoid foods high in saturated and trans - fats, such as red meat, whole milk products, and pastries.
Limit alcohol consumption to no more than 2 drinks per day for a man or 1 drink per day for a woman.
Eat less than 6 g of salt or
Physical ActivityReduced physical activity is a major risk factor for CVD. In elderly individuals, the risk of MI is reduced by as much as 50% by walking 30 minutes daily.[77, 78] A study of the associations between physical activity and risk of cardiovascular disease among 44,551 middle-aged men found vigorous- and moderate-intensity activity were associated with lower risk of disease.[174] On the other hand, the Cooper Center Longitudinal Study found that low fitness in mid-life was associated with higher lifetime risk for CVD death.[79]
Abnormal heart rate recovery (HRR) has been shown to predict mortality. A study by Jolly et al to determine whether HRR could be improved with cardiac rehabilitation suggests it can improve after patients with abnormal HRR at baseline normalize HRR with exercise. The mortality rate was similar to that of individuals with baseline normal HRR.[80]
The following general principles need to be considered in recommending increased physical activity:
Increased physical activity begins with increasing lifestyle activities, such as walking.A complete exercise program includes aerobic exercise, resistive training, and stretching.More frequent exercise, optimally daily, provides more benefit.More strenuous exercise, such as jogging, provides more benefit. A good goal is 75% of age-predicted maximal heart rate (220 - age of individual). Excellent benefit can be derived from 30 minutes of daily exercise.Studies have also shown that even 15 minutes a day or 90 minutes a week of moderate-intensity exercise may be beneficial.[81] The most recent scientific statement from the American Heart Association provides recommendations on implementing the most efficacious and effective physical activity and dietary strategies in adults.[82] European studies suggest that elevated waist circumference and physical inactivity are associated with an increased risk of coronary heart disease.[83] SmokingOf all the lifestyle modifications recommended to prevent CVD, smoking cessation is the most important. Tobacco use prematurely kills 435,000 Americans annually. Smoking cessation is the most cost-effective preventive measure, estimated at $220 per year of life saved. Individuals aged 30 years gain 3-5 years of life by stopping smoking and the mortality benefit was equally impressive in elderly populations.[84, 85] The most effective smoking cessation programs involve programmatic and/or group support and the use of nicotine substitutes and antidepressants, such as bupropion. Varenicline is a recent addition to the armamentarium and has been found to be superior to bupropion in this respect.[86, 87, 88]
Smoking is a risk factor for CVD in women and men; however, a systemic review and meta-analysis by Huxley and Woodward suggests that in some countries, smoking by women is on the rise; the study suggests that proper counseling and nicotine addiction programs should focus on young women.[89]
Smoking cessation counseling with supportive contact after a patient with acute myocardial infarction is discharged is potentially cost-effective and may reduce the incidence of smoking and further adverse health events.[90]
Secondary prevention (after development of CHD)Table 15. Smoking Cessation and Mortality After MI[91] (Open Table in a new window)
StudyPatients Studied (No.)5-Year Mortality RateQuittersSmokersSparrow, 1978365 (269 men, 96 women)12%25%Aberg, 1983Daly, 1983
983 (men only)
498 (men only)
16%
20%
22%
30%
Johansson, 1985
Perkins, 1985
156 (women only)
119 (90 men, 29 women)
15%
21%
27%
47%
Hedback, 1987305 (258 men, 47 women)16%31%
Several large observational studies, all of which had at least 5 years of follow-up and a meta-analysis including these studies, showed a substantial reduction in mortality [RR: 0.64 (I: 0.58-0.71)] in patients with a history of MI, CABG, angioplasty, or known CHD, who quit smoking compared with patients who continued to smoke.[92] The overall mortality risk of smokers who quit decreases by 50% in the first couple of years and tends to approach that of nonsmokers in approximately 5-15 years of cessation of smoking.
Primary prevention should start with lifestyle modification, including weight management, diet, physical activity, and smoking cessation. Hormone therapy increases cardiovascular events in postmenopausal women. Estrogen alone increases stroke, but it does not alter CHD events.
AspirinTwo recently published meta-analyses showed that aspirin use (75-162 mg/d) decreases the occurrence of primary MI by 25-33% and has also been shown to decrease death due to vascular causes; these benefits are not gender specific.[93, 94] However, all benefits have to be balanced against the risk of GI bleeding. Low-dose aspirin therapy (75 mg/d) is therefore recommended for primary prevention in individuals with a 10-year Framingham coronary risk estimate greater than 10%, outweighing risks of gastrointestinal hemorrhage and hemorrhagic stroke.[95] Aspirin has been shown to be similarly efficacious in secondary prevention of MI, stroke, and death secondary to vascular causes.[96, 97] However, a study by Berger et al suggests aspirin has only modest benefit in patients without clinical cardiovascular disease and this benefit is offset by its risk.[98]
PreviousNextClassification of RecommendationsRecommendations made herein are based largely on major practice guidelines from the National Institutes of Health and ACC/AHA. The information presented is adapted from recent statements by the AHA/ACC, which involved the process of partial adaptation of other guideline statements and reports and supplemental literature searches.[99]
The American College of Cardiology Foundation (ACCF) and the American Heart Association (AHA) have produced guidelines for the procedures of detection, management, or prevention of disease.[100]
Classification of recommendations and level of evidenceClassification of recommendations is as follows:
Class I - Conditions for which there is evidence and/or general agreement that a given procedure or treatment is beneficial, useful, and effective Class II - Conditions for which there is conflicting evidence and/or a divergence of opinion about the usefulness/efficacy of a procedure or treatment Class IIa - Weight or evidence/opinion is in favor or usefulness/efficacyClass IIb - Usefulness/efficacy is less well established by evidence/opinion Class III - Conditions for which there is evidence and/or general agreement that a procedure/treatment is not useful/effective and in some cases may be harmfulLevel of evidence is as follows:
Level of evidence A - Data derived from multiple randomized clinical trials or meta-analysesLevel of evidence B - Data derived from single randomized trial or nonrandomized studiesLevel of evidence C - Only consensus opinion or experts, case studies, or standard-of-careTable 16. Applying Classification of Recommendations and level of Evidence (in ACC/AHA format) (Open Table in a new window)
Size of Treatment Effect Class IBenefit >>> Risk
Procedure / treatment
should be
performed / administered.
Class IIa
Benefit >> Risk
(Additional studies with focused objectives needed)
Performing procedure / administering treatment is reasonable.
Class IIb
Benefit ≥ Risk
(Additional studies with broad objectives needed; additional registry data would be helpful)
Procedures / treatment may be considered.
Class III
Risk > Benefit
(No additional studies needed)
Procedure / treatment should not be performed / administered since it is not helpful and may be harmful.
Estimate
of
Certainty
(Precision)
of
Treatment
Effect
level A
Multiple (3-5) population risk strata evaluated*
General consistency of direction and magnitude of effect
Recommendation that procedure or treatment is useful/effective
Sufficient evidence from multiple randomized trials or meta-analyses
Recommendation in favor of treatment or procedure being useful/effective
Some conflicting evidence from multiple randomized trials or meta-analyses
Recommendation's usefulness / efficacy less well established
Greater conflicting evidence from multiple randomized trials or meta-analyses
Recommendation that procedure or treatment is not useful/effective and may be harmful
Sufficient evidence from multiple randomized trials or meta-analyses
level B
Limited (2-3) population risk strata evaluated*
Recommendation that procedure or treatment is useful / effective
Limited evidence from single randomized trial or nonrandomized studies
Recommendation in favor of treatment or procedure being useful / effective
Some conflicting evidence from single randomized trials or nonrandomized studies
Recommendation's usefulness / efficacy less well established
Greater conflicting evidence from single randomized trial or nonrandomized studies
Recommendation that procedure or treatment is not useful/effective and may be harmful
Limited evidence from single randomized trial or nonrandomized studies
level C
Very limited (1-2) population risk strata evaluated*
Recommendation that procedure or treatment is useful/effective
Only expert opinion, case studies, or standard-of-care
Recommendation in favor of treatment or procedure being useful/effective
Only diverging expert opinion, case studies, or standard-of-care
Recommendation's usefulness / efficacy less well established
Only diverging expert opinion, case studies, or standard-of-care
Recommendation that procedure or treatment is not useful/effective and may be harmful
Only expert opinion, case studies, or standard-of-care
Suggested phrases for writing recommendationsShould
Is recommended
Is indicated
Is useful / effective / beneficial
Is reasonable
Can be Useful / effective / beneficial
Is probably recommended or indicated
May/might be considered
May/might be reasonable
Usefulness / effectiveness is unknown / unclear / uncertain or not well established
Is not recommended
Is not indicated
Should not
Is not useful / effective / beneficial
May be harmful
*Data available from clinical trials or registries about the usefulness/efficacy in different subpopulations, such as gender, age, diabetes, history of prior MI, history of heart failure, and prior aspirin use. PreviousNextSecondary Prevention Goals and Management
Patients covered by these guidelines include those with established coronary and other atherosclerotic vascular disease, including peripheral arterial disease, atherosclerotic aortic disease, and carotid artery disease. Treatment for patients whose only manifestation of cardiovascular risk is diabetes will be the topic of a separate AHA scientific statement.
The AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients With Coronary and Other Atherosclerotic Vascular Disease: 2011 Update: A Guideline From the American Heart Association and American College of Cardiology Foundation has been released.[101]
Smoking cessationThe goal is complete cessation and no exposure to environmental tobacco smoke.
Ask the patient about tobacco use status at every visit. I (B)Advise every patient who uses tobacco to quit. I (B)Assess the patient’s willingness to quit using tobacco. I (B)Assist the patient by counseling and developing a plan for quitting. I (B)Arrange follow-up, referral to special programs, or pharmacotherapy (including nicotine replacement and bupropion). I (B)Urge the patient to avoid exposure to environmental tobacco smoke at work and home. I (B)Blood pressure controlThe goal is BP
For all patients, initiate or maintain lifestyle modification, weight control, increased physical activity, alcohol moderation, sodium reduction, and increased consumption of fresh fruits, vegetables, and low-fat dairy products. I (B)
For patients with BP ≥140/90 mm Hg (or 130/80 mm Hg for individuals with chronic kidney disease or diabetes), as tolerated, add BP medication, treating initially with beta-blockers and/or ACE inhibitors, with addition of other drugs, such as thiazides, as needed to achieve goal blood pressure. I (A)
DietDiets that include nonhydrogenated unsaturated fats as the predominant form of dietary fat, whole grains as the primary form of carbohydrate, fruits and vegetables, omega-3 fatty acids (from fish, fish oil supplements, or plant sources) offer significant protection against coronary heart disease.
Light-to-moderate alcohol consumption (5-25 g/d) has been significantly associated with a lower incidence of cardiovascular and all-cause mortality in patients with cardiovascular disease. A meta-analysis by Costanzo et al found J-shaped curves for alcohol consumption and mortality, with a significant maximal protection against cardiovascular mortality with consumption of approximately 26 g/d and maximal protection against mortality from any cause in the range of 5-10 g/d.[102]
Lipid managementThe goal is LDL cholesterol
The following measures should be taken for all patients:
Start dietary therapy. Reduce the intake of saturated fats (to I (B)Adding plant stanol/sterols (2 g/d) and viscous fiber (>10 g/d) will further lower LDL cholesterol level.Promote daily physical activity and weight management. I (B)Encourage increased consumption of omega-3 fatty acids in the form of fish or in capsule form (1 g/d) for risk reduction. (Pregnant and lactating women should limit their intake of fish to minimize exposure to methylmercury.) For treatment of elevated triglyceride levels, higher doses are usually necessary for risk reduction. IIb (B)Assess fasting lipid profile in all patients and within 24 hours of hospitalization for those with an acute cardiovascular or coronary event. For hospitalized patients, initiate lipid-lowering medication as recommended below before discharge according to the following schedule:
LDL cholesterol level should be I (A)Further reduction of LDL cholesterol level to IIa (A)If baseline LDL cholesterol level is 100 mg/dL, initiate LDL-lowering drug therapy. I (A)If the patient is on treatment and LDL cholesterol is 100 mg/dL, intensify LDL-lowering drug therapy (may require LDL-lowering drug combination [standard dose of statin with ezetimibe, bile acid sequestrant, or niacin]). I (A)If baseline LDL cholesterol level is 70-100 mg/dL, treating to LDL cholesterol level of IIa (B)If triglyceride levels are 200-499 mg/dL, non-HDL cholesterol level should be I (B)Further reduction of non-HDL cholesterol level to IIa (B)Therapeutic options to reduce non-HDL cholesterol level are as follows:
More intense LDL cholesterol-lowering therapy, I (B)Niacin (after LDL cholesterol–lowering therapy), IIa (B)Fibrate therapy (after LDL cholesterol–lowering therapy), IIa (B)If triglyceride levels are 500 mg/dL, therapeutic options to prevent pancreatitis are fibrate or niacin before LDL-lowering therapy, and treat LDL cholesterol level to goal after triglyceride-lowering therapy. Achieve non-HDL cholesterol level of I (C) (Patients with very high triglycerides should not consume alcohol. The use of bile acid sequestrant is relatively contraindicated when triglycerides are >200 mg/dL.) (The combination of high-dose statin plus fibrate can increase risk for severe myopathy. Statin doses should be kept relatively low with this combination. Dietary supplement niacin must not be used as a substitute for prescription niacin.)
In 2011, The National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health stopped a clinical trial studying a blood lipid treatment that was adding high-dose, extended-release niacin to statin treatment in people with heart and vascular disease.[103] The study was stopped because the treatment did not reduce the risk of cardiovascular events, including heart attacks and stroke. The AIM HIGH study selected patients at risk for cardiovascular events despite well-controlled LDL ("bad cholesterol"). Participants who took high-dose, extended-release niacin and statin treatment had increased HDL cholesterol and lower triglyceride levels compared with participants who took a statin alone; however, but the combination treatment did not reduce fatal or nonfatal heart attacks, strokes, hospitalizations for acute coronary syndrome, or revascularization procedures to improve blood flow in the arteries of the heart and brain.
Further, The AIM HIGH investigators concluded that patients with atherosclerotic cardiovascular disease and LDL cholesterol levels of less than 70 mg/dL (1.81 mmol/L) experienced no incremental clinical benefit from the addition of niacin to statin therapy, despite significant improvements in HDL cholesterol and triglyceride levels.[104]
A study by Mills et al suggests intensive statin dosing reduces the risk of nonfatal events (coronary heart disease and nonfatal myocardial infarction ) and may have a role in reducing mortality.[105] However, the benefits of high-dose statins must be weighed against the risk of myopathy, including rhabdomyolysis, at high doses.
When LDL-lowering medications are used, obtain at least a 30-40% reduction in LDL cholesterol levels. If LDL cholesterol 50% in LDL cholesterol levels by either satins or LDL cholesterol-lowering drug combinations.
RVX-208, the first oral agent designed to enhance apolipoprotein (apo) A-I synthesis, has shown to increase apoA-I, HDL-C, and concentration of large HDL particles, as well as increase in liver enzymes.[106]
Lowering LDL cholesterol with statin regimens may have an effect in people with moderate-to-severe kidney disease.[107] The Study of Heart and Renal Protection (SHARP) Trial suggests simvastatin (20 mg) plus ezetimibe (10 mg) daily safely reduces the incidence of major atherosclerotic events in a wide range of patients with advanced chronic kidney disease.
Secondary prevention trials in older persons with CAD and hypercholesterolemia have demonstrated that statin drugs reduced all-cause mortality, cardiovascular mortality, coronary events, coronary revascularization, stroke, and intermittent claudication. Statin therapy significantly decreases cardiovascular events and all-cause mortality in both women and men.[108]
Raal et al found that lipid-lowering therapy is associated with delayed cardiovascular events and prolonged survival in patients with homozygous familial hypercholesterolemia.[109]
Physical activityThe goal of physical activity is 30 minutes, 7 days per week (minimum 5 d/w). The US guidelines for physical activity suggest low, moderate, and high activity levels. A meta-analysis by Sattlemair et al attempted to quantify these amounts and found that "some physical activity is better than none" and "additional benefits occur with more physical activity."[110]
For all patients, assess risk with a physical activity history and/or an exercise test to guide prescription. I (B)For all patients, encourage 30-60 minutes of moderate-intensity aerobic activity (eg, brisk walking) on most, preferably all, days of the week, supplemented by an increase in daily lifestyle activities (eg, walking breaks at work, gardening, household work). I (B)Encourage resistance training 2 days per week. IIb (C)Advise medically supervised programs for high-risk patients (eg, recent acute coronary syndrome or revascularization, heart failure). I (B)Weight managementThe goal of weight management is body mass index of 18.5-24.9 kg/m2 and waist circumference of [111]
Assess body mass index and/or waist circumference on each visit and consistently encourage weight maintenance or reduction through an appropriate balance of physical activity, caloric intake, and formal behavioral programs when indicated to maintain or achieve a body mass index between 18.5 and 24.9 kg/m2. I (B)If waist circumference (measured horizontally at the iliac crest) is 35 inches in women and 40 inches in men, initiate lifestyle changes and consider treatment strategies for metabolic syndrome as indicated. I (B)The initial goal of weight loss therapy should be to reduce body weight by approximately 10% from baseline. With success, further weight loss can be attempted if indicated through further assessment. I (B)According to The Aerobics Center Longitudinal Study, maintaining or improving fitness is associated with a lower risk of all-cause and CVD mortality in men. Health care providers should encourage men to exercise regularly, regardless of age, as it is important for longevity regardless of BMI change.[112]
Diabetes managementThe goal of diabetes management is to maintain glycosylated hemoglobin (HbA1c) concentration of
Initiate lifestyle and pharmacotherapy to achieve near-normal HbA1c level. I (B)Begin vigorous modification of other risk factors (eg, physical activity, weight management, BP control, and cholesterol management) as recommended above. I (B)Coordinate diabetic care with the patient's primary care physician or endocrinologist. I (C)Antiplatelet agents and anticoagulantsStart aspirin 75-162 mg/d, and continue indefinitely in all patients unless contraindicated. I (A) For patients undergoing coronary artery bypass grafting, aspirin should be started within 48 hours after surgery to reduce saphenous vein graft closure. Dosing regimens ranging from 100-325 mg/d appear to be efficacious. Doses higher than 162 mg/d can be continued for up to 1 year. I (B)Start and continue clopidogrel 75 mg/d in combination with aspirin for up to 12 months in patients after acute coronary syndrome or percutaneous coronary intervention with stent placement (at least 1 month, but ideally 12 months, for bare metal stent; at least 12 months for drug-eluting stents). I (B) Patients who have undergone percutaneous coronary intervention with stent placement should initially receive higher-dose aspirin at 162-325 mg/d for 1 month for bare metal stent, 3 months after sirolimus-eluting stent, 6 months after paclitaxel-eluting stent, after which daily long-term aspirin use should be continued indefinitely at a dose of 75-162 mg.[113] I (B)Manage warfarin to international normalized ratio of 2.0-3.0 for paroxysmal or chronic atrial fibrillation or flutter, and in post–MI patients when clinically indicated (eg, atrial fibrillation, left ventricular thrombus). I (A)Use of warfarin in conjunction with aspirin and/or clopidogrel is associated with increased risk of bleeding and should be monitored closely. I (B)A nationwide cohort study suggests NSAID treatment duration in patients with prior myocardial infarction, whether short term or long term, is associated with increased risk of death and recurrent myocardial infarction in patients with prior myocardial infarction and is not recommended for this population.[114] NSAID use should be limited from a cardiovascular safety point of view. Renin, angiotensin, and aldosterone system blockersConsider the following with ACE inhibitors:
Start and continue indefinitely in all patients with left ventricular ejection fraction ≥40% and in those with hypertension, diabetes, or chronic kidney disease, unless contraindicated. I (A)Consider for all other patients. I (B)Among lower-risk patients with normal left ventricular ejection fraction in whom cardiovascular risk factors are well controlled and revascularization has been performed, use of ACE inhibitors may be considered optional. IIa (B)Consider the following with angiotensin receptor blockers:
Use in patients who are intolerant of ACE inhibitors and have heart failure or have had an MI with left ventricular ejection fraction ≤40%. I (A)Consider in other patients who are intolerant of ACE inhibitors. I (B)Consider use in combination with ACE inhibitors in systolic dysfunction heart failure. IIb (B)Aldosterone blockade are used in post-MI patients without significant renal dysfunction (creatinine should be >2.5 mg/dL in men and > 2.0 mg/dL in women) or hyperkalemia (potassium should be [115] I (A)
Beta-blockersStart and continue indefinitely in all patients who have had MI, ACS, or LV dysfunction with or without heart failure symptoms, unless contraindicated. l (A)Consider chronic therapy for all other patients with coronary or other vascular disease or diabetes, unless contraindicated. lla (C)Influenza vaccinationPatients with cardiovascular disease should have an influenza vaccination. I (B)
PreviousNextWomen and Coronary Artery DiseaseIn the United States, CHD is the leading cause of death in both men and women, claiming more lives than cancer, accidents, and diabetes combined.[116, 117] Although breast cancer may be more feared, age-adjusted death rates from CVD in women are 4 times higher in white women and 6 times higher in black women than the death rates for breast cancer.
The 2010 ACCF/AHA report on assessment of cardiovascular risk in asymptomatic adults includes the recommendation that for all adult women and men, global risk scoring should be performed and a family history of cardiovascular disease should be obtained for cardiovascular risk assessment.[10]
Compared with men, LDL cholesterol is lower and HDL cholesterol is higher in women before menopause. Although women have lower rates of hypertension and cigarette smoking than men, rates for obesity and diabetes mellitus are higher. Diabetes mellitus is a particularly serious risk factor in women, tripling the risk of cardiovascular death and causing diabetic women to have the same frequency of CVD as diabetic men.[118, 119, 120] HDL cholesterol and triglyceride levels are more predictive of CVD in women than in men.[121] Women have been noted to have similar or slightly higher prevalence of stable angina as compared to men.[122]
It is now known that women tend to present more commonly with unstable angina as compared to men, the reverse of which is true for MI. However, when women do present with MI, they are more likely to have Q wave rather than non-Q wave.[123, 124] Mortality rates of MI and CABG are about 50% higher in women, mostly related to older age of onset. Lipid lowering has shown similar efficacy in women and men in the angiographic progression and event trials. Cardioprotective agents, including aspirin, beta-blockers, and ACE inhibitors, appear to have similar efficacy in men and women.[125, 126, 127]
Hormone therapy is no longer recommended to prevent coronary events in postmenopausal women with or without established CHD. Although hormone therapy improves LDL and HDL cholesterol levels[128, 129] , it also increases coagulation and inflammation (as measured by C-reactive protein [CRP]) and decreases LDL particle size.[130, 4] Treatment rates for risk factors in women tend to be even lower than in men, as are rates for coronary angiography and coronary artery revascularization following presentation with chest pain.
Women who may have had radiotherapy through the mid-1980s to treat breast cancer are also at an increased risk of mortality from cardiovascular disease. The concern is even greater if the woman was treated for a left-sided breast cancer with contemporary tangential breast or chest wall radiotherapy.[131]
Finally, it must be emphasized that while the guidelines detailed above represent best practice, their formulation is often a blend of science and art. Therefore, guideline interpretation should always occur alongside good clinical judgment.
Previous Contributor Information and DisclosuresAuthorTamam N Mohamad, MD Fellow, Department of Cardiology, Wayne State University, Detroit Medical Center
Tamam N Mohamad, MD is a member of the following medical societies: American College of Cardiology, American College of Physicians-American Society of Internal Medicine, American Medical Association, Michigan State Medical Society, and National Arab American Medical Association
Disclosure: Nothing to disclose.
Luis C Afonso, MD Assistant Professor, Department of Internal Medicine-Cardiology, Program Director of Cardiology Fellowship Program, Wayne State University; Director of Echocardiography Laboratory, Harper University Hospital
Luis C Afonso, MD is a member of the following medical societies: American College of Cardiology, American College of Physicians, American Medical Association, and American Society of Echocardiography
Disclosure: Nothing to disclose.
Pretti Ramappa, MD Fellow, Department of Cardiology, Detroit Medical Center, Wayne State University
Pretti Ramappa, MD is a member of the following medical societies: American College of Cardiology and American College of Physicians
Disclosure: Nothing to disclose.
Pawan Hari, MD, MPH Resident Physician, Department of Internal Medicine, Wayne State University School of Medicine
Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Medscape Salary Employment
Brian Olshansky, MD Professor of Medicine, Department of Internal Medicine, University of Iowa College of Medicine
Brian Olshansky, MD is a member of the following medical societies: American College of Cardiology, American Heart Association, Cardiac Electrophysiology Society, and Heart Rhythm Society
Disclosure: Guidant/Boston Scientific Honoraria Speaking and teaching; Medtronic Honoraria Speaking and teaching; Guidant/Boston Scientific Consulting fee Consulting; BioControl Consulting fee Consulting; Boehringer Ingelheim Consulting fee Consulting; Amarin Consulting fee Review panel membership; sanofi aventis Review panel membership
Amer Suleman, MD Private Practice
Amer Suleman, MD is a member of the following medical societies: American College of Physicians, American Heart Association, American Institute of Stress, American Society of Hypertension, Federation of American Societies for Experimental Biology, Royal Society of Medicine, and Society of Cardiac Angiography and Interventions
Disclosure: Nothing to disclose.
Yasmine Subhi Ali, MD, MSCI, FACC, FACP President, Nashville Preventive Cardiology, PLLC; Assistant Clinical Professor of Medicine, Vanderbilt University School of Medicine
Yasmine Subhi Ali, MD, MSCI, FACC, FACP is a member of the following medical societies: American College of Cardiology, American College of Physicians, American Heart Association, American Medical Association, National Lipid Association, and Tennessee Medical Association
Disclosure: Nothing to disclose.
National Center for Health Statistics (NCHS). Compressed mortality file: underlying cause of death, 1979 to 2005. Centers for Disease Control. Available at http://wonder.cdc.gov/mortSQL.html.
Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. Feb 17 1998;97(6):596-601.
Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. May 24 1997;349(9064):1498-504. [Medline].
American Heart Association. Heart Disease and Stroke Statistics - 2009 Update. Available at http://www.americanheart.org/presenter.jhtml?identifier=3000090.
Weintraub WS, Daniels SR, Burke LE, et al. Value of Primordial and Primary Prevention for Cardiovascular Disease: A Policy Statement From the American Heart Association. Circulation. Aug 23 2011;124(8):967-990. [Medline].
Strasser T. Reflections on cardiovascular diseases. Interdisciplinary Science Review. 1978;3:225-30.
Ebrahim S, Taylor F, Ward K, Beswick A, Burke M, Davey Smith G. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst Rev. Jan 19 2011;CD001561. [Medline].
Pande RL, Perlstein TS, Beckman JA, Creager MA. Secondary prevention and mortality in peripheral artery disease: national health and nutrition examination study, 1999 to 2004. Circulation. Jul 5 2011;124(1):17-23. [Medline].
National Heart, Lung, and Blood Institute (NHLBI). Estimate of 10-Year Risk for Coronary Heart Disease Framingham Point Scores. Available at http://www.nhlbi.nih.gov/guidelines/cholesterol/risk_tbl.htm.
Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. Dec 14 2010;56(25):2182-99. [Medline].
MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. Jul 6 2002;360(9326):7-22. [Medline].
Balagopal PB, de Ferranti SD, Cook S, et al. Nontraditional Risk Factors and Biomarkers for Cardiovascular Disease: Mechanistic, Research, and Clinical Considerations for Youth: A Scientific Statement From the American Heart Association. Circulation. Jun 14 2011;123(23):2749-2769. [Medline].
Berry JD, Dyer A, Cai X, et al. Lifetime risks of cardiovascular disease. N Engl J Med. Jan 26 2012;366(4):321-9. [Medline].
Rozanski A, Gransar H, Shaw LJ, et al. Impact of Coronary Artery Calcium Scanning on Coronary Risk Factors and Downstream Testing The EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) Prospective Randomized Trial. J Am Coll Cardiol. Apr 12 2011;57(15):1622-32. [Medline].
Yusuf S, Lonn E, Bosch J. Lipid lowering for primary prevention. Lancet. Apr 4 2009;373(9670):1152-5. [Medline].
Hedner T, Hansson L, Jern S. What is happening to blood pressure?. Blood Press. May 1996;5(3):132-3. [Medline].
Sjol A, Thomsen KK, Schroll M. Secular trends in blood pressure levels in Denmark 1964-1991. Int J Epidemiol. Aug 1998;27(4):614-22. [Medline].
Burt VL, Cutler JA, Higgins M, Horan MJ, Labarthe D, Whelton P, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991. Hypertension. Jul 1995;26(1):60-9. [Medline].
Teo KK, Ounpuu S, Hawken S, Pandey MR, Valentin V, Hunt D, et al. Tobacco use and risk of myocardial infarction in 52 countries in the INTERHEART study: a case-control study. Lancet. Aug 19 2006;368(9536):647-58. [Medline].
Wang TD, Chen WJ, Chien KL, Seh-Yi Su SS, Hsu HC, Chen MF, et al. Efficacy of cholesterol levels and ratios in predicting future coronary heart disease in a Chinese population. Am J Cardiol. Oct 1 2001;88(7):737-43. [Medline].
National Heart, Lung, and Blood Institute (NHLBI). ATP III Update 2004: Implications of Recent Clinical Trials for the ATP III Guidelines. NIH. Available at http://www.nhlbi.nih.gov/guidelines/cholesterol/atp3upd04.pdf.
Ridker PM, Genest J, Boekholdt SM, Libby P, Gotto AM, Nordestgaard BG, et al. HDL cholesterol and residual risk of first cardiovascular events after treatment with potent statin therapy: an analysis from the JUPITER trial. Lancet. Jul 31 2010;376(9738):333-9. [Medline].
Bulbulia R, Bowman L, Wallendszus K, Parish S, Armitage J, Peto R, et al. Effects on 11-year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20,536 high-risk individuals: a randomised controlled trial. Lancet. Dec 10 2011;378(9808):2013-20. [Medline].
Koenig W, Ridker PM. Rosuvastatin for primary prevention in patients with European systematic coronary risk evaluation risk = 5% or Framingham risk >20%: post hoc analyses of the JUPITER trial requested by European health authorities. Eur Heart J. Jan 2011;32(1):75-83. [Medline]. [Full Text].
Blaha MJ, Budoff MJ, DeFilippis AP, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet. Aug 20 2011;378(9792):684-92. [Medline].
O'Brien T, Dinneen SF, O'Brien PC, Palumbo PJ. Hyperlipidemia in patients with primary and secondary hypothyroidism. Mayo Clin Proc. Sep 1993;68(9):860-6. [Medline].
Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. Feb 28 2000;160(4):526-34. [Medline].
Crippin JS, Lindor KD, Jorgensen R, Kottke BA, Harrison JM, Murtaugh PA, et al. Hypercholesterolemia and atherosclerosis in primary biliary cirrhosis: what is the risk?. Hepatology. May 1992;15(5):858-62. [Medline].
Matzkin VB, Geissler C, Coniglio R, Selles J, Bello M. Cholesterol concentrations in patients with Anorexia Nervosa and in healthy controls. Int J Psychiatr Nurs Res. Jan 2006;11(2):1283-93. [Medline].
Mordasini R, Klose G, Greten H. Secondary type II hyperlipoproteinemia in patients with anorexia nervosa. Metabolism. Jan 1978;27(1):71-9. [Medline].
Zavaroni I, Dall'Aglio E, Alpi O, Bruschi F, Bonora E, Pezzarossa A, et al. Evidence for an independent relationship between plasma insulin and concentration of high density lipoprotein cholesterol and triglyceride. Atherosclerosis. Jun 1985;55(3):259-66. [Medline].
Kalkhoff RK, Kim HJ. The influence of hormonal changes of pregnancy on maternal metabolism. Ciba Found Symp. Mar 30-Apr 1 1978;29-56. [Medline].
Facchini FS, Hollenbeck CB, Jeppesen J, Chen YD, Reaven GM. Insulin resistance and cigarette smoking. Lancet. May 9 1992;339(8802):1128-30. [Medline].
Lipids and lipoproteins in symptomatic coronary heart disease. Distribution, intercorrelations, and significance for risk classification in 6,700 men and 1,500 women. The Bezafibrate Infarction Prevention (BIP) Study Group, Israel. Circulation. Sep 1992;86(3):839-48. [Medline].
Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. May 1983;67(5):968-77. [Medline].
Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. Dec 17 2002;106(25):3143-, Primary and Secondary Prevention of Coronary Artery Disease






0 comments:
Post a Comment