Most sudden cardiac deaths in the United States are caused by ventricular tachycardia (VT) or ventricular fibrillation (VF), at an estimated rate of approximately 300,000 deaths per year. Ventricular tachycardia refers to any rhythm faster than 100 beats per minute, with 3 or more irregular beats in a row, arising distal to the bundle of His. The rhythm may arise from working ventricular myocardium and/or from the distal conduction system.
Essential update: Safety and efficacy of complete endocardial VT substrate ablation after MIComplete endocardial ventricular tachycardia substrate ablation (CEVTSA) is safe and effective in patients with previous myocardial infarction (MI), even in those in whom VT substrate has not been identified, according to a study of 59 post-myocardial infarction patients by Arenal and colleagues. Dense scar area and VT cycle length were significant independent predictors of VT recurrence.[1, 2]
Signs and symptomsHistory
The symptoms of ventricular tachycardia include the following:
PalpitationLight-headednessSyncopeChest painAnxietyPhysical examination
During VT, the following symptoms may be observed:
HypotensionTachypneaSigns of diminished perfusion: Including a diminished level of consciousness, pallor, and diaphoresisHigh jugular venous pressureCannon a waves: If the atria are in sinus rhythmVariation in intensity of first heart sound: Due to loss of atrioventricular (AV) synchronyFollowing conversion, physical findings during normal sinus rhythm are related to any underlying structural heart disease.
VT can also result in sudden death. Patients in whom this occurs may first present with syncope.
See Clinical Presentation for more detail.
DiagnosisAssess levels of serum electrolytes, including the following, in all patients with VT:
Calcium: Ionized calcium levels are preferred over total serum calcium levelsMagnesiumPhosphateHypokalemia, hypomagnesemia, and hypocalcemia may predispose patients to either monomorphic VT or torsade de pointes.
Laboratory studies can also include the following:
levels of therapeutic drugs, such as digoxinToxicology screens: May be helpful in those cases related to recreational drug useSerum cardiac troponin I or T levels or other cardiac markers: To evaluate for myocardial ischemia or infarctionVT at acute presentation
In patients who have VT at acute presentation and who are unconscious or hemodynamically unstable, the diagnosis is made from the physical findings and electrocardiogram (ECG) rhythm strip.
If circumstances allow, a full 12-lead electrocardiogram should be obtained prior to urgent cardioversion.
Laboratory studies are impractical, and advanced cardiac life support (ACLS) protocols must be quickly followed. However, in patients who have VT at acute presentation and are hemodynamically stable, a 12-lead ECG and electrolytes may be obtained prior to attempted conversion with medications or sedation and cardioversion.
VT postconversion
In patients with VT postconversion, diagnosis proceeds as follows:
Repeat the ECG after termination of VTInclude electrolyte levels in an acute evaluationPerform toxicology screens for cocaine metabolites and tricyclic antidepressants: In accordance with the patient’s clinical history Check cardiac enzyme levels: If clinical symptoms or signs of ischemia are presentPerform echocardiography and coronary angiography: Following conversion to sinus rhythm, to assess for structural and ischemic heart diseaseElectrophysiologic study
Diagnostic electrophysiologic study (EPS) requires placement of electrode catheters in the ventricle, followed by programmed ventricular stimulation using progressive pacing protocols. EPS is particularly relevant in patients who are felt to be at high risk for sudden death due to significant underlying structural heart disease.
See Workup for more detail.
ManagementMedications
The mainstays of treatment for clinically stable VT are the various antidysrhythmic drugs. Intravenous medications are used to suppress acute monomorphic VT; in the United States, these are limited to the following agents:
ProcainamideLidocaineAmiodaroneBeta-adrenergic blocking agents metoprolol, esmolol, and propranololICDs
American College of Cardiology/American Heart Association/European Society of Cardiology (ACC/AHA/ESC) guidelines recommend implantable cardioverter-defibrillator (ICD) therapy for primary prevention to reduce total mortality by a reduction in sudden cardiac death (SCD) in patients with the following characteristics[3] :
Left ventricular (LV) dysfunction due to previous myocardial infarction (MI)At least 40 days post-MILV ejection fraction (LVEF) of 30-40% or lessNew York Heart Association (NYHA) functional class II or IIIReceiving chronic optimal medical therapyReasonably expected to survive with good functional status for more than 1 yearAblation
Endocardial catheter ablation is used early in idiopathic, monomorphic VT (ie, VT in a structurally normal heart) but can also be used to reduce arrhythmia burden in the presence of cardiomyopathy.
See Treatment and Medication for more detail.
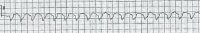
Image library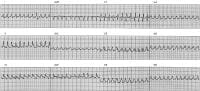 This is a rapid monomorphic ventricular tachycardia (VT), 280 beats per minute, associated with hemodynamic collapse. This tracing was obtained from a patient with severe ischemic cardiomyopathy during an electrophysiologic (EP) study. The rhythm later converted to sinus with a single external shock. This patient had an atrial rate of 72 beats per minute (measured with intracardiac electrodes, not shown). Although ventriculoatrial dissociation (faster V rate than A rate) is diagnostic of VT, the surface ECG findings (dissociated P waves, fusion or capture beats) are only present approximately 20% of the time. In this tracing, the ventricular rate is simply too fast for P waves to be observed. VT with cycle lengths from 200-240 ms is often termed ventricular flutter. NextBackground
This is a rapid monomorphic ventricular tachycardia (VT), 280 beats per minute, associated with hemodynamic collapse. This tracing was obtained from a patient with severe ischemic cardiomyopathy during an electrophysiologic (EP) study. The rhythm later converted to sinus with a single external shock. This patient had an atrial rate of 72 beats per minute (measured with intracardiac electrodes, not shown). Although ventriculoatrial dissociation (faster V rate than A rate) is diagnostic of VT, the surface ECG findings (dissociated P waves, fusion or capture beats) are only present approximately 20% of the time. In this tracing, the ventricular rate is simply too fast for P waves to be observed. VT with cycle lengths from 200-240 ms is often termed ventricular flutter. NextBackgroundVentricular tachycardia (VT) refers to any rhythm faster than 100 (or 120) beats per minute arising distal to the bundle of His. The rhythm may arise from working ventricular myocardium and/or from the distal conduction system. (See Etiology.) Go to Pediatric Ventricular Tachycardia for complete information on this topic.
VT may be reflected in symptoms such as syncope, palpitations, and dyspnea. It is often, but not always, associated with hemodynamic compromise, particularly if the left ventricle is impaired or the heart rate is especially fast. With some exceptions, VT is associated with increased risk of sudden death. (See Etiology, Prognosis, History, Physical Examination, Workup.)
VT generally is a consequence of ischemic or structural heart disease or electrolyte deficiencies (eg, hypokalemia, hypocalcemia, hypomagnesemia). It can also be triggered by the following (see Etiology):
Use of sympathomimetic agents (from intravenous inotropes to illicit drugs such as methamphetamine or cocaine)Systemic diseases that affect the myocardium, such as sarcoidosis, systemic lupus erythematosus, hemochromatosis, and rheumatoid arthritisOther structural congenital disorders, such as right ventricular dysplasia and tetralogy of FallotDigitalis toxicity - Can lead to biventricular tachycardia.Inherited channelopathies[4] Drugs that prolong the QT complex (eg, type 1A antidysrhythmics, droperidol and related phenothiazines)Drugs that prolong the QT complex may cause torsade de pointes. (See Etiology.)
Monomorphic and polymorphic ventricular tachycardiaVT may be monomorphic (originating from a single focus with identical QRS complexes) or polymorphic (may appear as an irregular rhythm, with varying QRS amplitudes and morphology). Examples of monomorphic and polymorphic VTs are seen below.
 This is a rapid monomorphic ventricular tachycardia (VT), 280 beats per minute, associated with hemodynamic collapse. This tracing was obtained from a patient with severe ischemic cardiomyopathy during an electrophysiologic (EP) study. The rhythm later converted to sinus with a single external shock. This patient had an atrial rate of 72 beats per minute (measured with intracardiac electrodes, not shown). Although ventriculoatrial dissociation (faster V rate than A rate) is diagnostic of VT, the surface ECG findings (dissociated P waves, fusion or capture beats) are only present approximately 20% of the time. In this tracing, the ventricular rate is simply too fast for P waves to be observed. VT with cycle lengths from 200-240 ms is often termed ventricular flutter.
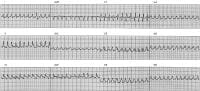
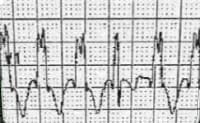
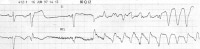
This is a rapid monomorphic ventricular tachycardia (VT), 280 beats per minute, associated with hemodynamic collapse. This tracing was obtained from a patient with severe ischemic cardiomyopathy during an electrophysiologic (EP) study. The rhythm later converted to sinus with a single external shock. This patient had an atrial rate of 72 beats per minute (measured with intracardiac electrodes, not shown). Although ventriculoatrial dissociation (faster V rate than A rate) is diagnostic of VT, the surface ECG findings (dissociated P waves, fusion or capture beats) are only present approximately 20% of the time. In this tracing, the ventricular rate is simply too fast for P waves to be observed. VT with cycle lengths from 200-240 ms is often termed ventricular flutter. 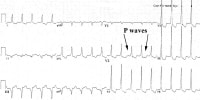 This is a slow monomorphic ventricular tachycardia (VT), 121 beats per minute, from a patient with an old inferior wall myocardial infarction and well-preserved left ventricular function (ejection fraction [EF] 55%). He presented with symptoms of palpitation and neck fullness. Note the ventriculoatrial dissociation, most obvious in V2 and V3. Slower VT rates and preserved left ventricular (LV) function are associated with a better long-term prognosis.
This is a slow monomorphic ventricular tachycardia (VT), 121 beats per minute, from a patient with an old inferior wall myocardial infarction and well-preserved left ventricular function (ejection fraction [EF] 55%). He presented with symptoms of palpitation and neck fullness. Note the ventriculoatrial dissociation, most obvious in V2 and V3. Slower VT rates and preserved left ventricular (LV) function are associated with a better long-term prognosis. 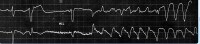 Polymorphic ventricular tachycardia. Sustained and nonsustained ventricular tachycardia
Polymorphic ventricular tachycardia. Sustained and nonsustained ventricular tachycardiaNonsustained VT is defined as a run of tachycardia of less than 30 seconds duration; longer runs are considered sustained VT.
While nonsustained ventricular tachycardia is a frequently observed dysrhythmia, sustained, monomorphic ventricular tachycardia is uncommon in the emergency department (ED) setting due to aggressive treatment of myocardial ischemia.
When sustained VT causes signs or symptoms of diminished perfusion, emergent treatment is necessary.
Electrocardiography in ventricular tachycardiaNo absolute electrocardiographic criteria exist for establishing the presence of VT. However, several factors suggest VT, including the following:
Rate greater than 120 beats per minute (usually 150-200)Wide QRS complexes (>140 ms; see the ECG below)Presence of atrioventricular (AV) dissociationFusion beatsCapture beats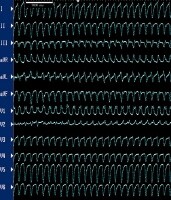 This patient is a 64-year-old man with a history of prior myocardial infarction and syncope. In patients with prior myocardial infarction, the most common mechanism of wide QRS complex tachycardia is ventricular tachycardia. Myocardial scar tissue in ventricular tachycardia
This patient is a 64-year-old man with a history of prior myocardial infarction and syncope. In patients with prior myocardial infarction, the most common mechanism of wide QRS complex tachycardia is ventricular tachycardia. Myocardial scar tissue in ventricular tachycardiaThe most common setting for VT is ischemic heart disease, in which myocardial scar tissue is the substrate for electrical reentry, but it can be seen in other conditions that create myocardial scar tissue, such as ion channel abnormalities, dilated cardiomyopathies, hypertrophic cardiomyopathy, right ventricular dysplasia, Chagas disease,[5] and surgical incisions in the ventricle.
Ventricular tachycardia versus ventricular fibrillationVT is distinguished from ventricular fibrillation (VF), which is a grossly disorganized, rapid ventricular rhythm that varies in interval and waveform. VF may be difficult to distinguish from rapid, polymorphic VT. There is a potential definitional overlap with accelerated idioventricular rhythm when an automatic VT is noted from 100-120 beats per minute.
Sudden death accounts for approximately half of all deaths from cardiovascular disease and is generally caused by VT and VF.
PreviousNextPathophysiologyRegardless of the arrhythmia mechanism in ventricular tachycardia (VT), the severity of clinical symptoms determines the urgency with which VT must be treated.
During VT, cardiac output is reduced due to the rapid heart rate and lack of a properly timed or coordinated atrial contraction. Ischemia and mitral[6] insufficiency may also contribute to hemodynamic intolerance. Hemodynamic collapse is more likely when underlying left ventricular dysfunction is present or with very rapid rates. Diminished cardiac output may result in diminished myocardial perfusion, worsening inotropic response and degeneration to VF, resulting in sudden death.
In patients with monomorphic VT, mortality risk correlates with the degree of structural heart disease. Underlying structural heart diseases, such as ischemic cardiomyopathy, dilated cardiomyopathy, hypertrophic cardiomyopathy, Chagas disease, and right ventricular dysplasia, have all been associated with monomorphic or polymorphic VT degenerating to VF.[5]
Even without such degeneration, VT can also produce congestive heart failure and hemodynamic compromise, with subsequent morbidity and mortality.
If VT is hemodynamically tolerated, the incessant tachyarrhythmia may cause a dilated cardiomyopathy. This may develop over a period of weeks to months and resolves with successful management of the VT.[7] A similar course is occasionally seen with ventricular bigeminy, despite the absence of sustained high rates.
PreviousNextEtiologyVentricular tachycardia (VT) is usually a consequence of structural or ischemic heart disease, with breakdown of normal conduction patterns. Abnormal automaticity (which tends to favor ectopic foci) or activation of reentrant pathways in the myocardium can exist to generate the dysrhythmia. Electrolyte disturbances, ischemia, and sympathomimetics may increase the likelihood of VT in the susceptible myocardium.
Atrioventricular dissociationAV dissociation, shown in the ECGs below, is apparent in approximately half of VT episodes, and when present, it is a hallmark characteristic of VT.[8] This occurs because the sinus node is depolarizing the atria at a rate that is slower than the pathologic, faster ventricular rate. P waves can be visualized at times in between or embedded in the QRS complexes, but the P waves and QRS complexes have their own independent rates.
 This ECG shows another form of idiopathic ventricular tachycardia, seen in the absence of structural heart disease. This rhythm arises from the left ventricular septum and often responds to verapamil. Upon superficial examination, it appears to be a supraventricular tachycardia with bifascicular conduction block (RBBB/LAFB). Closer examination of lead V1 shows narrowing of the fourth QRS complex, consistent with fusion between the wide QRS complex and a conducted atrial beat, confirming AV dissociation and VT mechanism.
This ECG shows another form of idiopathic ventricular tachycardia, seen in the absence of structural heart disease. This rhythm arises from the left ventricular septum and often responds to verapamil. Upon superficial examination, it appears to be a supraventricular tachycardia with bifascicular conduction block (RBBB/LAFB). Closer examination of lead V1 shows narrowing of the fourth QRS complex, consistent with fusion between the wide QRS complex and a conducted atrial beat, confirming AV dissociation and VT mechanism. 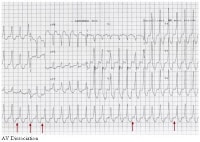 AV dissociation. Fusion and capture beats
AV dissociation. Fusion and capture beatsFusion beats and capture beats can occur in the presence of VT, depending on the refractory period of the AV node and the timing of ventricular and atrial depolarizations, respectively.
A fusion beat has a mixed morphology, due to normal AV node/His-Purkinje conduction occurring simultaneously with abnormal (a wide, complex QRS) ventricular depolarization. A normally conducted impulse travels from the AV node through the normal conduction pathway (a narrow QRS), and the competing impulse originates from the abnormal ectopic ventricular focus outside of the normal conduction pathway (a wide QRS). The two converge, leading to a mixed (fused) QRS.
A capture beat occurs when an atrial impulse arrives at the AV node at a "fortuitous" time, when the AV node has just recovered from its refractory period. The timing has to be just right, as the AV node is frequently in its refractory state due to depolarization caused by retrograde conduction from the rapid ventricular rhythm. When this occurs, conduction will proceed normally through the AV node/His-Purkinje system, "capturing" the ventricle and leading to a normal, narrow QRS complex. Fusion beats, capture beats, and AV dissociation are shown in the image below.
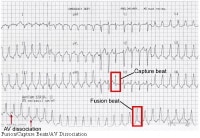 Fusion beats, capture beats, and AV dissociation.
Fusion beats, capture beats, and AV dissociation. Retrograde conduction can also exist from the ventricles to the atria via the AV node. This is not AV dissociation and reveals itself in an electrocardiogram (ECG) as a 1:1 correlation between the wide QRS complex and an inverted P wave, which follows the QRS complex.
Monomorphic ventricular tachycardiaWhen the ventricular activation sequence is constant, the electrocardiographic pattern remains the same, and the rhythm is called monomorphic VT (seen in the ECG below).
 Monomorphic ventricular tachycardia.
Monomorphic ventricular tachycardia. Monomorphic VT is most commonly seen in patients with underlying structural heart disease. There is typically a zone of slow conduction, most commonly due to scarring and/or fibrillar disarray. Causes include prior infarct, any primary cardiomyopathy, surgical scar, hypertrophy, and muscle degeneration.
Reentrant tachycardias occur when an electrical wavefront travels slowly through the zone of slow conduction (usually damaged muscle protected by scar tissue), allowing the rest of the circuit time to repolarize. The wavefront breaks out of the scar, activates the ventricle, and reenters the slow conduction zone. The QRS morphology during VT can be used to predict the exit site from the zone of slow conduction.[9]
Although most patients with VT have underlying structural heart abnormalities, monomorphic VT is occasionally observed in patients with structurally normal hearts (idiopathic VT). These VTs are often exercise dependent, and their clinical behavior may be more consistent with triggered activity or abnormal automaticity.
Monomorphic VTs are typically named for their site of origin. The most commonly involved sites are the right ventricular outflow tract, left ventricular outflow tract, left ventricular septum, and aortic root.[10]
Although monomorphic VTs have classically been considered benign, sudden death may occur, albeit rarely, despite the presence of a structurally normal heart.[11]
Polymorphic ventricular tachycardiaWhen the QRS complex varies from beat to beat, the rhythm is described as polymorphic VT and suggests a variable electrical activation sequence. The most notorious, and probably the most common, form of polymorphic VT is torsade de pointes. The disorder’s name is a French term that suggests a "twisting of the points" of the QRS complexes over time
Torsade de pointes has unusual shifting-axis QRS complexes that appear (on ECGs) as if the heart is rotating upon an axis. It typically occurs during sinus rhythm and in the presence of drugs or conditions that prolong the QT interval (eg, type 1A antiarrhythmics, hypomagnesemia, droperidol). The dysrhythmia may occur either in the presence or in the absence of myocardial ischemia or infarction. Examples of torsade de pointes are shown below.
 Torsade de pointes. This is a polymorphic ventricular tachycardia (VT) associated with resting QT-interval prolongation. In this case, it was caused by the potassium channel blocker, sotalol. This rhythm is also observed in families with mutations affecting certain cardiac ion channels.
Torsade de pointes. This is a polymorphic ventricular tachycardia (VT) associated with resting QT-interval prolongation. In this case, it was caused by the potassium channel blocker, sotalol. This rhythm is also observed in families with mutations affecting certain cardiac ion channels. 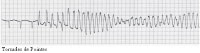 Torsades de pointes.
Torsades de pointes. The term torsade de pointes is reserved for polymorphic VT observed in the setting of a prolonged QT interval. Other polymorphic VTs are occasionally observed during ischemia or myocarditis.
Acquired QT prolongation is observed with certain potassium channel–blocking medications. Most of the causative drugs block the delayed rectifier cardiac potassium current, IKr. These agents include quinidine, erythromycin, haloperidol, and many others.
Congenital long QT syndrome is a group of genetic disorders involving abnormal cardiac ion channels (most commonly potassium channels responsible for ventricular repolarization).
In acquired and congenital long QT syndromes, prolonged repolarization predisposes to torsade de pointes, which is most likely a reentrant rhythm with a constantly varying circuit. Other inherited ion channel abnormalities may cause idiopathic VF and familial polymorphic VT in the absence of QT prolongation.
Go to Torsade de Pointes for complete information on this topic.
Sustained and nonsustained ventricular tachycardiaThe most common cause of sustained, monomorphic VT is a prior myocardial infarction (MI) with ventricular myocardial scar formation. The presence of myocardial fibrosis is a substrate for slow conduction pathways and associated reentry mechanisms.
Nonsustained VT and ectopy result from abnormal automaticity mechanisms and are more commonly associated with acute myocardial ischemia.
Idioventricular rhythmA second variant of VT is accelerated idioventricular rhythm. Sometimes termed slow ventricular tachycardia, this dysrhythmia presents with a rate of 60-100 beats per minute. It typically occurs with underlying heart disease (ischemic or structural), is transient, and only rarely is associated with hemodynamic compromise or collapse. Treatment of the dysrhythmia itself usually is not required unless significant hemodynamic impairment develops.
Inherited dysrhythmiaDue to advances in molecular biology, a number of inherited dysrhythmic disorders with a propensity toward VT have been described. Brugada syndrome, congenital long and short QT syndromes, and catecholaminergic polymorphic VT have autosomal dominant inheritance patterns.[12, 13, 14, 15] Mechanistically, each disorder is characterized by imbalanced ion transport across the cardiac cellular membrane, which leads to abnormalities in cardiac repolarization and, consequently, increased risk of dysrhythmia. An autosomal recessive form of long QT syndrome is associated with increased arrhythmia risk and congenital hearing loss.
These syndromes have all been linked to sudden cardiac death. Patients with these disorders are managed with a combination of genetic typing, antidysrhythmic medications, lifestyle modification, and, in selected cases, implantable cardioverter-defibrillator (ICD) placement.[16]
Supraventricular tachycardiaWide complex conduction during supraventricular tachycardia can mimic VT. The 2 most common forms of are (1) AV reentrant tachycardia (AVRT) and (2) AV nodal reentrant tachycardia with aberrant conduction (AVNRT).
AVRT can be either orthodromic or antidromic depending on the direction of conduction through the AV node. All antidromic AVRTs cause wide-complex tachycardia due to ventricular activation outside of the His-Purkinje system, and some orthodromic AVRTs conduct with wide QRS complexes as a result of functional or preexisting bundle-branch block or intraventricular conduction delay. Note the images below.
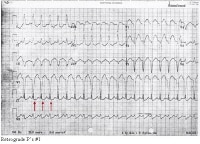 Retrograde P's #1
Retrograde P's #1 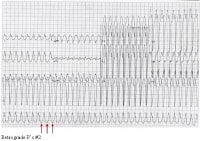 Retrograde P's #2.
Retrograde P's #2. Aberrantly conducted SVT circuits can mimic VT, but careful ECG analysis can allow discrimination of VT from aberrant SVT in most cases. See Electrocardiography for details.
Risk factors for ventricular tachycardiaTriggers of VT include electrolyte abnormalities, ischemia, inflammation, and sleep apnea.
Hypokalemia is the most important arrhythmia trigger clinically, followed by hypomagnesemia. Hyperkalemia may also predispose to VT and VF, particularly in patients with structural heart disease.
Certain genetic groups carry genetically mediated risk of unusual heart disease. Examples include the Veneto region of Italy and Greek island of Naxos (right ventricular dysplasia),[17] and northeastern Thailand (idiopathic ventricular fibrillation/Brugada syndrome).[18]
Ventricular tachycardia risk within populations generally varies with the risk factors for atherosclerosis, rather than ethnic differences per se.
Among patients younger than 35 years, the most common causes of sudden death, and presumably of VT, include hypertrophic cardiomyopathy, right ventricular cardiomyopathy, myocarditis, and long QT syndrome.
Risk factors for VT also include the following:
Use of sympathomimetic agents - From intravenous inotropes to illicit agents such as methamphetamine or, as previously mentioned, cocaine Drugs that prolong the QT complex (eg, type 1A antidysrhythmics, droperidol and related phenothiazines) - May infrequently cause torsade de pointes Systemic diseases that affect the myocardium, such as sarcoidosis, systemic lupus erythematosus, hemochromatosis, and rheumatoid arthritis Structural congenital disorders such as right ventricular dysplasia and tetralogy of FallotDigitalis toxicity - Can lead to biventricular tachycardiaInherited channelopathies[4]The American College of Cardiology/American Heart Association / European Society of Cardiology (ACC/AHA/ESC) 2006 guidelines (the most current version available as of May 18, 2011) for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death recommend an antidigitalis antibody for patients with sustained ventricular arrhythmias, advanced AV block, and/or asystole caused by digitalis toxicity.[3]
PreviousNextEpidemiologyIncidence and mortality rate in the United StatesThe incidence of ventricular tachycardia (VT) in the United States is not well quantified because of the clinical overlap of VT with ventricular fibrillation (VF).
Examination of sudden death data provides a rough estimate of VT incidence. Most sudden cardiac deaths are caused by VT or VF, at an estimated rate of approximately 300,000 deaths per year in the United States, or about half of the estimated cardiac mortality in this country.
A prospective surveillance study gave a sudden death incidence of 53 per 100,000, accounting for 5.6% of all mortality.[19] This is only a rough estimate of VT incidence, because many patients have nonfatal VT and because arrhythmic sudden deaths may be associated with VF or bradycardia rather than with VT.
In patients with ischemic cardiomyopathy and nonsustained VT, sudden death mortality rates approach 30% in 2 years.
International incidence of ventricular tachycardiaVentricular tachycardia and coronary artery disease are common throughout most of the developed world. In developing countries, ventricular tachycardia and other heart diseases are relatively less common.
Sex predilectionVentricular tachycardia (VT) is observed more frequently in men, because ischemic heart disease is more prevalent among men. Among patients with coronary artery disease in the Framingham Heart Study, male deaths were more common than female deaths (46% vs 34%, respectively).[20]
Females with acquired or congenital long QT syndromes are at greater risk for sudden death. The opposite is true for arrhythmogenic right ventricular dysplasia (a 2-fold male predominance) and Brugada syndrome (an approximately 8-fold male predominance).
As coronary artery disease (CAD) becomes more common in women, it seems certain that the incidence of VT in women will increase.
Age predilectionThe incidence of ischemic ventricular tachycardia (VT) increases with age, regardless of sex, as the prevalence of coronary artery disease increases.
VT is unusual among pediatric patients, although when present, it occurs in the postoperative cardiac setting or in patients with associated congenital heart disease. Tachydysrhythmias in this population generally are paroxysmal supraventricular tachycardias (PSVTs).
Ventricular tachycardia incidence rates peak in the middle decades of life, following the incidence of structural heart disease.
Idiopathic VT can be observed at any age.
Go to Pediatric Ventricular Tachycardia for complete information on this topic.
Morbidity and mortality in ventricular tachycardiaMorbidity and mortality in VT arise principally from spontaneous degeneration into the more malignant VF. (See Pathophysiology, above.) In patients with ischemic cardiomyopathy and nonsustained VT, sudden death mortality rates approach 30% in 2 years.
If VT is associated with hemodynamic collapse, morbidity in resuscitated survivors can include ischemic encephalopathy, acute renal insufficiency, transient ventricular dysfunction, aspiration pneumonitis, and trauma related to resuscitative efforts.
PreviousNextPrognosisPrognosis in ventricular tachycardia (VT) varies with the specific cardiac process but is predicted best by left ventricular function.
As previously mentioned, in patients with ischemic cardiomyopathy and nonsustained VT, sudden-death mortality rates approach 30% in 2 years.
In patients with idiopathic VT, the prognosis is excellent, and the major risk is due to poorly timed syncopal spells.
A few exceptions exist to the left-ventricle rule. Patients with long QT syndrome, right ventricular dysplasia, and hypertrophic cardiomyopathy may be at increased risk of sudden death despite relatively preserved left ventricular function. These possibilities should be considered in any patient with a strong family history of premature sudden death.
PreviousNextPatient EducationFor patient education information, see the Heart Center, as well as Heart Rhythm Disorders, Supraventricular Tachycardia, and Palpitations.
PreviousProceed to Clinical Presentation , Ventricular Tachycardia





0 comments:
Post a Comment