Exercise testing is a cardiovascular stress test that uses treadmill bicycle exercise with electrocardiography (ECG) and blood pressure monitoring.[1] Pharmacologic stress testing, established after exercise testing, is a diagnostic procedure in which cardiovascular stress induced by pharmacologic agents is demonstrated in patients with decreased functional capacity or in patients who cannot exercise. Pharmacologic stress testing is used in combination with imaging modalities such as radionuclide imaging and echocardiography.[2, 3]
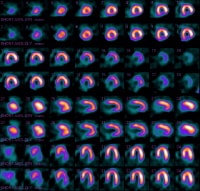
Exercise stress testing, which is now widely available at a relatively low cost, is currently used most frequently to estimate prognosis and determine functional capacity, to assess the probability and extent of coronary disease, and to assess the effects of therapy. Ancillary techniques, such as metabolic gas analysis, radionuclide imaging (see the images below), and echocardiography, can provide further information that may be needed in selected patients, such as those with moderate or prior risk.
 Normal radionuclide uptake (dipyridamole-Cardiolite).
Normal radionuclide uptake (dipyridamole-Cardiolite).  Normal wall motion with radionuclide uptake.
Normal wall motion with radionuclide uptake. Cardiovascular exercise stress testing in conjunction with ECG has been established as one of the focal points in the diagnosis and prognosis of cardiovascular disease, specifically coronary artery disease (CAD).[4, 5]
Exercise physiologyThe initiation of dynamic exercise results in increases in ventricular heart rate, stroke volume, and cardiac output as a result of vagal withdrawal and sympathetic stimulation. Alveolar ventilation and venous return also increase as a consequence of sympathetic vasoconstriction. The overall hemodynamic response depends on the amount of muscle mass involved, exercise efficiency, conditioning, and exercise intensity.
In the initial phases of exercise in the upright position, cardiac output is increased by an augmentation in stroke volume mediated through the use of the Frank-Starling mechanism and heart rate. The increase in cardiac output in the later phases of exercise is due primarily to an increase in ventricular rate.
During strenuous exertion, sympathetic discharge is maximal and parasympathetic stimulation is withdrawn, resulting in autoregulation with generalized vasoconstriction, except in the vital organs (cerebral and coronary circulations).
Release of venous and arterial norepinephrine from sympathetic postganglionic nerve endings is increased, and epinephrine levels are increased at peak exertion, resulting in a rise in ventricular contractility. As exercise progresses, skeletal muscle blood flow increases; oxygen extraction increases as much as 3-fold; peripheral resistance decreases; and systolic blood pressure (SBP), mean arterial pressure, and pulse pressure usually increase. Diastolic blood pressure (DBP) remains unchanged or may increase or decrease by approximately 10 mm Hg.
The pulmonary vascular bed can accommodate as much as a 6-fold increase in cardiac output, with only modest increases in pulmonary arterial pressure, pulmonary capillary wedge pressure, and right atrial pressure; this is not a limiting determinant of peak exercise capacity in healthy subjects.
Maximum heart rate and cardiac output are decreased in older individuals, in part because of decreased beta-adrenergic responsiveness. Maximum heart rate can be calculated by subtracting the patient’s age (in years) from 220 (standard deviation, 10-12 beats/min).
The age-predicted maximum heart rate is a useful measurement for safety purposes and for estimating the adequacy of the stress to evoke inducible ischemia. A patient who reaches 80% of the age-predicted maximum is considered to have a good test result, and an age-predicted maximum of 90% or better is considered excellent.
In the postexercise phase, hemodynamics return to baseline within minutes after exercise is discontinued. The return of vagal stimulation is an important cardiac deceleration mechanism after exercise; it is more pronounced in well-trained athletes but is blunted in patients with chronic congestive heart failure.
Intense physical work or important cardiorespiratory impairment may interfere with achievement of a steady state, and an oxygen deficit occurs during exercise. The oxygen debt is the total oxygen uptake in excess of the resting oxygen uptake during the recovery period.
NextIndications and ContraindicationsTreadmill stress testing is indicated for diagnosis and prognosis of cardiovascular disease, specifically CAD. Contraindications have been outlined in guidelines from the American College of Cardiology (ACC) and the American Heart Association (AHA).
Absolute contraindications include the following:
Acute myocardial infarction (MI; within 2 days)Unstable angina not previously stabilized by medical therapy – Appropriate timing of tests depends on the level of risk of unstable angina as defined by the Agency for Health Care Policy and Research Unstable Angina Guidelines Uncontrolled cardiac arrhythmias causing symptoms or hemodynamic compromiseSymptomatic severe aortic stenosisUncontrolled symptomatic heart failureAcute pulmonary embolus or pulmonary infarctionAcute myocarditis or pericarditisAcute aortic dissectionRelative contraindications can be superseded if the benefits of exercise outweigh the risks. They include the following:
Left main coronary stenosisModerate stenotic valvular heart diseaseElectrolyte abnormalitiesSevere arterial hypertension – In the absence of definite evidence, the committee suggests an SBP higher than 200 mm Hg, a DBP higher than 110 mm Hg, or both Tachyarrhythmias or bradyarrhythmiasHypertrophic cardiomyopathy and any other forms of outflow tract obstructionMental or physical impairment leading to an inability to exercise adequatelyHigh-degree atrioventricular (AV) blockThe vast majority of treadmill exercise tests are performed on adults with symptoms of known or probable ischemic heart disease. Candidates for exercise stress testing may have stable symptoms of chest pain, may be stabilized by medical therapy after experiencing symptoms of unstable chest pain, or may have already had an MI or undergone a vascularization procedure.
The clinical suggestion of CAD on the basis of patient history findings, ECG tracings, and symptoms of chest pain must be established and used as a guide to determine if treadmill exercise testing may be useful according to the Bayes theorem, which states that the diagnostic power of exercise stress testing is maximal when the pretest probability of CAD is intermediate (30-70%) as indicated by age, sex, and nature of chest pain.
When the diagnosis of CAD is confirmed on the basis of age, sex, description of chest pain, and history of previous MI, a clinical need may arise for risk or prognostic assessment to reach a decision regarding possible coronary angiography or revascularization to guide further medical management.
MI (see the images below) is a common first presentation of ischemic heart disease. This subset of patients also may require prognostic or risk assessment.
 Inferior-wall myocardial infarct and fixed defect.
Inferior-wall myocardial infarct and fixed defect.  Motion abnormalities in inferior wall consistent with inferior-wall myocardial infarction.
Motion abnormalities in inferior wall consistent with inferior-wall myocardial infarction. 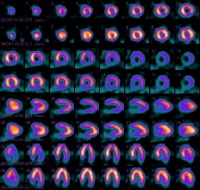 Inferobasal fixed defect and lateral wall ischemia.
Inferobasal fixed defect and lateral wall ischemia.  Wall motion abnormalities in inferobasal region. PreviousNextTechnical ConsiderationsBest practices
Wall motion abnormalities in inferobasal region. PreviousNextTechnical ConsiderationsBest practicesThe ACC/AHA guidelines for exercise stress testing were initially developed in 1997 to create recommendations for the appropriate use of testing in the diagnosis, prognosis, and treatment of patients with known or probable cardiovascular disease.[6] These guidelines were revised in 2002.[7]
In the original guidelines, the available scientific evidence was not ranked as belonging to level A, B, or C. In the later recommendations that appear in the update, however, the level of evidence is considered.
Evidence is ranked highest (A) if the data are based on multiple randomized clinical trials involving large numbers of patients. An intermediate rank (B) indicates data derived from a limited number of randomized trials involving small numbers of patients or from careful analyses of nonrandomized studies or observational registries. The lowest rank (C) indicates that the recommendation is primarily based on expert consensus. When few or no data exist, this is noted in the text.
ACC/AHA classes I, II, and III are used to categorize indications for exercise stress testing; they include the following:
Class I – Conditions for which evidence and/or general agreement exists that a given procedure or treatment is useful and effective Class II – Conditions for which conflicting evidence and/or a divergence of opinion exists concerning the usefulness or efficacy of a procedure or treatment; this class is further divided into subclasses IIa and IIb Class IIa – The weight of evidence/opinion is in favor of usefulness/efficacyClass IIb – Usefulness/efficacy is less well established by evidence/opinionClass III – Conditions for which evidence and/or general agreement exists that the procedure/treatment is not useful/effective and, in some cases, may be harmful Complication preventionExercise testing is a well-established procedure that has been in widespread clinical use for decades. Although it is generally safe, both myocardial infarction and death have been reported and can be expected to occur at a rate of 1 incident per 2500 tests. Therefore, it is vital to use good clinical judgment when deciding which patients should undergo exercise testing.
Factors that are important in establishing good clinical outcomes from exercise testing include the following:
The quality, expertise, and experience of the professional and technical staff performing and interpreting the study (to reduce observer error) The sensitivity, specificity, and accuracy of the technique (to establish limitations of this procedure)The cost and accuracy of the technique as compared with more expensive imaging procedures (to establish the risk-to-benefit ratio, to determine the effect of positive or negative results on clinical decision making, and, to weigh the potential psychological benefits of patient reassurance) PreviousProceed to Periprocedural Care , Treadmill Stress Testing





0 comments:
Post a Comment