Signs and symptoms of prosthetic heart valve malfunction depend on the type of valve, its location, and the nature of the complication. Presentations may include the following:
Acute prosthetic valve failure: Sudden onset of dyspnea, syncope, or precordial painAcute aortic valve failure: Sudden death; survivors have acute severe dyspnea, sometimes accompanied by precordial pain, or syncope Subacute valvular failure: Symptoms of gradually worsening congestive heart failure; they also may present with unstable angina or, at times, may be entirely asymptomatic Embolic complications: Symptoms related to the site of embolization (eg, stroke, myocardial infarction [MI], sudden death, or symptoms of visceral or peripheral embolization) Anticoagulant-related hemorrhage: Symptoms related to the site of hemorrhageA history of fever should raise the possibility of prosthetic valve endocarditis (PVE).
On physical examination, normal prosthetic heart valve sounds include the following:
Mechanical valves: Loud, high-frequency, metallic closing sound; soft opening sound (tilting disc and bileaflet valves); low-frequency opening and closing sounds of nearly equal intensity (caged ball valves) Tissue valves: Closing similar to those of native valves, low-frequency early opening sound in the mitral positionProsthetic heart valve murmurs noted include the following:
Aortic prosthetic valves: Some degree of outflow obstruction with a resultant systolic ejection murmur (loudest in caged ball and small porcine valves); low-intensity diastolic murmur (tilting disc and bileaflet valves) Mitral prosthetic valves: Low-grade systolic murmur (caged ball valves); short diastolic murmur (bioprostheses and, occasionally, St. Jude bileaflet valves)Additional findings may include the following:
Acute valvular failure: Evidence of poor tissue perfusion; hyperdynamic precordium and right ventricular impulse (50% of cases); absence of a normal valve closure sound or presence of an abnormal regurgitant murmur Subacute valvular failure: Rales and jugular venous distention; signs of right-side failure; a new regurgitant murmur or absence of normal closing sounds; a new or worsening hemolytic anemia (may be the only presenting abnormality) PVE (often obscure): Fever (97% of cases); a new or changing murmur (56% of cases); classic signs of native valve endocarditis; splenomegaly; congestive heart failure, septic shock, or primary valvular failure; systemic emboliSee Clinical Presentation for more detail.
DiagnosisLaboratory studies that may be useful include the following:
Complete blood countBlood urea nitrogen (BUN) and creatinine levelsUrinalysisBlood cultureProthrombin time (PT) or international normalized ratio (INR)Imaging studies that may be helpful include the following:
Chest radiography: This can help in delineating the valvular morphology and determining whether the valve and occluder are intact; each of the most commonly used valve types has its own characteristic radiographic appearance Echocardiography (2-dimensional, Doppler, transesophageal [the study of choice for a suspected prosthetic valve complication], transthoracic) Cinefluorography: This may detect impaired occluder movement but often cannot readily determine the etiologyComputed tomography: A consensus statement from the Society of Cardiovascular Computed Tomography (SCCT) states that CT should be performed as part of the evaluation of all patients being considered for transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR), except those in whom CT is contraindicated,  [1, 2] and that the CT images should be interpreted with a member of the TAVI/TAVR team or reviewed with the operator before the procedureSee Workup for more detail.
ManagementIn patients with acute valvular failure, diagnostic studies must be performed simultaneously with resuscitative efforts.
Treatment approaches to primary valve failure include the following:
Emergency valve replacementConcomitant adjunctive therapyAfterload reduction and inotropic supportIn selected cases, intra-aortic balloon counterpulsationTreatment approaches to PVE include the following:
Intravenous antibiotics administered as soon as 2 sets of blood cultures are drawnCessation of warfarin until central nervous system involvement is ruled out and invasive procedures are determined to be unnecessary[3] Consideration of anticoagulationConsideration of emergency surgery in patients with moderate to severe heart failure or with an unstable prosthesis noted on echocardiography or fluoroscopyTreatment approaches to thromboembolic complications include the following:
Anticoagulation (if it has not already been initiated or if the patient has a subtherapeutic INR)Assessment of valve functionNote: US dabigatran prescribing information now includes a contraindication in patients with mechanical prosthetic valves[4]Treatment approaches to prosthetic valve thrombosis include the following:
Surgery (historically the mainstay of treatment but associated with a high mortality)Thrombolytic therapy (appropriate for selected patients with thrombosed prosthetic valves): Should always be performed in conjunction with cardiovascular surgical consultation In cases of major anticoagulant-related hemorrhage, reversal of anticoagulationSee Treatment and Medication for more detail.
Image library St. Jude Medical mechanical heart valve. Photograph courtesy of St. Jude Medical, Inc. All rights reserved. St. Jude Medical is a registered trademark of St. Jude Medical, Inc. NextBackground
St. Jude Medical mechanical heart valve. Photograph courtesy of St. Jude Medical, Inc. All rights reserved. St. Jude Medical is a registered trademark of St. Jude Medical, Inc. NextBackgroundImplantation of prosthetic cardiac valves to treat hemodynamically significant valvular disease has become an increasingly common procedure. It is estimated that more than 60,000 patients per year are undergoing heart valve replacement in the United States. Replacement of diseased valves reduces the morbidity and mortality associated with native valvular disease but comes at the expense of risking complications related to the implanted prosthetic device. These complications include primary valve failure, prosthetic valve endocarditis (PVE), prosthetic valve thrombosis (PVT), thromboembolism, and mechanical hemolytic anemia. In addition, because many of these patients require long-term anticoagulation, anticoagulant-related hemorrhage may occur.
Transcatheter approaches to aortic valve implantation have allowed patients previously felt to be poor operative risks to undergo valve replacement.
Emergency physicians must be able to rapidly identify patients at risk and begin appropriate diagnostic testing, stabilization, and treatment. Even when promptly recognized and treated, acute prosthetic valve failure is associated with a high mortality rate.
More than 80 models of artificial valves have been introduced since 1950. In day-to-day emergency practice, however, it is necessary to be familiar with a few basic types. Prosthetic valves are either created from synthetic material (mechanical prosthesis) or fashioned from biological tissue (bioprosthesis).
Three main designs of mechanical valves exist: the caged ball valve, the tilting disc (single leaflet) valve, and the bileaflet valve. The only Food and Drug Administration (FDA)–approved caged ball valve is the Starr-Edwards valve, shown in the image below.
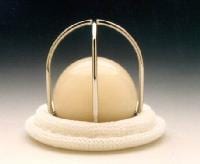 Starr-Edwards Silastic ball valve mitral Model 6120. Reproduced with permission from Baxter International, Inc.
Starr-Edwards Silastic ball valve mitral Model 6120. Reproduced with permission from Baxter International, Inc. Tilting disc valve models include the Medtronic Hall valve, shown in the image below, Omnicarbon (Medical CV) valves, Monostrut (Alliance Medical Technologies), and the discontinued Bjork-Shiley valves.
 Medtronic Hall mitral valve. Reproduced with permission from Medtronic, Inc.
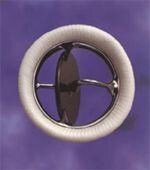
Medtronic Hall mitral valve. Reproduced with permission from Medtronic, Inc. Bileaflet valves include the St. Jude (St. Jude Medical), shown in the image below, which is the most commonly implanted valve in the United States; CarboMedics valves (Sulzer CarboMedics); ATS Open Pivot valves (ATS Medical); and On-X and Conform-X valves (MCRI).
 St. Jude Medical mechanical heart valve. Photograph courtesy of St. Jude Medical, Inc. All rights reserved. St. Jude Medical is a registered trademark of St. Jude Medical, Inc.
St. Jude Medical mechanical heart valve. Photograph courtesy of St. Jude Medical, Inc. All rights reserved. St. Jude Medical is a registered trademark of St. Jude Medical, Inc. Bioprosthetic (xenograft) valves are made from porcine valves or bovine pericardium. Porcine models include the Carpentier-Edwards valves (Edwards Lifesciences) and Hancock II and Mosaic valves (Medtronic); both valves are shown in the images below.
 Carpentier-Edwards Duralex mitral bioprosthesis (porcine). Reproduced with permission from Baxter International, Inc.
Carpentier-Edwards Duralex mitral bioprosthesis (porcine). Reproduced with permission from Baxter International, Inc.  The Hancock M.O. II aortic bioprosthesis (porcine). Reproduced with permission from Medtronic, Inc.
The Hancock M.O. II aortic bioprosthesis (porcine). Reproduced with permission from Medtronic, Inc. Pericardial valves include the Perimount series valves (Edwards LifeSciences). Ionescu-Shiley pericardial valves have been discontinued. More recently, stentless porcine valves have been used. They offer improved hemodynamics with a decreased transvalvular pressure gradient when compared with older stented models. These models include the Edwards Prima Plus, Medtronic Freestyle, and Toronto SPV valve (St. Jude Medical).[5]
Homografts or preserved human aortic valves are used in a minority of patients.
Two devices have been approved for transcatheter aortic valve implantation (TAVI): the SAPIEN XT valve (Edwards LifeSciences), made of bovine pericardium, and the CoreValve (Medtronic), made of porcine pericardium.
PreviousNextPathophysiologyValve failurePrimary valve failure may occur abruptly from the tearing or breakage of components or from a thrombus suddenly impinging on leaflet mobility. More commonly, valve failure presents gradually from calcifications or thrombus formation. Bioprostheses are less thrombogenic than mechanical valves, but this advantage is balanced by their diminished durability when compared with mechanical valves. Although 30-35% of bioprostheses will fail within 10-15 years, it can be anticipated that most mechanical valves will remain functional for 20-30 years.
Stenosis or incompetence of prosthetic valves occurs and may be due to a tear or perforation of the valve cusp, valvular thrombosis, pannus formation, valve calcification, or stiffening of the leaflets.
Primary failure of mechanical valves may be caused by suture line dehiscence, thrombus formation, or breakage or separation of the valve components. Acute valvular regurgitation or embolization of the valve fragments may result.
When the mitral valve acutely fails, rapid left atrial volume overload causes increased left atrial pressure. Pulmonary venous congestion and, ultimately, pulmonary edema occur. Cardiac output is decreased because a portion of the left ventricular output is being regurgitated into the left atrium. The compensatory mechanism of increased sympathetic tone increases the heart rate and the systemic vascular resistance (SVR). This may worsen the situation by decreasing diastolic filling time and impeding left ventricular outflow, thereby increasing the regurgitation.
Acute failure of a prosthetic aortic valve causes a rapidly progressive left ventricular volume overload. Increased left ventricular diastolic pressure results in pulmonary congestion and edema. The cardiac output is reduced substantially. The compensatory mechanism of an increased heart rate and a positive inotropic state, mediated by increased sympathetic tone, partly helps to maintain output. However, this is hampered by an increase in SVR, which impedes forward flow. Increased systolic wall tension causes a rise in myocardial oxygen consumption. Myocardial ischemia in acute aortic regurgitation may occur, even in the absence of coronary artery disease.
Biological prosthetic valves often slowly degenerate over time, become calcified, or suffer from thrombus formation. These events result in the slowly progressive failure of the valve. The presentation is usually that of gradually worsening congestive heart failure, with increasing dyspnea. Alternatively, patients may present with unstable angina or systemic embolization, or they may be entirely asymptomatic.
The first TAVI device for use in the United States was approved in November 2011. Subsequently, not enough time has passed to gather data concerning longevity and use. Vascular complications and strokes related to the procedure are decreasing with improved delivery techniques and equipment. Complications related to the conduction system requiring permanent pacemaker implantation occur in 14% of patients. This risk is increased with the use of the CoreValve prosthesis.[6]
Prosthetic valve endocarditisPVE occurring within 1 year of implantation (early PVE) usually is due to perioperative contamination or hematogenous spread. PVE occurring after 1 year (late PVE) is usually caused by hematogenous spread.[7]
The pathologic hallmark of PVE in mechanical valves is ring abscesses. Ring abscess may lead to valve dehiscence and perivalvular leakage. Local extension results in the formation of myocardial abscesses. Further extension to the conduction system often results in a new atrioventricular block. Valve stenosis and purulent pericarditis occur less frequently.
Bioprosthetic valve PVE usually causes leaflet tears or perforations. Valve stenosis is more common with bioprosthetic valves than with mechanical valves. Ring abscess, purulent pericarditis, and myocardial abscesses are much less frequent in bioprosthetic valve PVE.
Finally, glomerulonephritis, mycotic aneurysms, systemic embolization, and metastatic abscesses also may complicate PVE.
PreviousNextEpidemiologyFrequencyUnited States
Prosthetic valve thrombosis is more common in mechanical valves. With proper anticoagulation, the rate of thrombosis in all valves is within the range of 0.1-5.7% per patient-year. Caged ball valves have the highest rate of thromboembolic complications, and bileaflet valves have the lowest. Valve thrombosis is increased with valves in the mitral position and in patients with subtherapeutic anticoagulation.
Anticoagulant-related hemorrhagic complications of mechanical valves include major hemorrhage in 1-3% of patients per year and minor hemorrhage in 4-8% of patients per year. Low-grade hemolytic anemia occurs in 70% of prosthetic heart valve recipients, and severe hemolytic anemia occurs in 3%. The incidence is increased with caged ball valves and in those with perivalvular leaks. Primary valve failure occurs in 3-4% of patients with bioprostheses within 5 years of implantation and in up to 35% of patients within 15 years. Mechanical valves have a much lower incidence of primary failure. PVE occurs in 2-4% of patients. The incidence is 3% in the first postoperative year, then 0.5% for subsequent years. The incidence is higher when valve surgery is performed in patients with active native valve endocarditis. The incidence is higher in mitral valves. Mechanical and biological valves are equally susceptible to early PVE, but the incidence of late PVE is higher for bioprostheses. Despite improvements in surgical techniques, no appreciable change in the incidence has been observed.[8] Mortality/MorbidityAcute failure of a prosthetic aortic valve usually leads to sudden or near-sudden death. Prompt recognition and treatment of acute prosthetic mitral valve failure can be lifesaving.[7]
PVE has an overall mortality rate of 50%. In early PVE, the mortality rate is 74%. In late PVE, the mortality rate is 43%. The mortality rate with a fungal etiology is 93%. The mortality rate for staphylococcal infections is 86%. PVE due to Staphylococcus has a mortality rate of 25-40%.[7, 8] Fatal anticoagulant-induced hemorrhage occurs in 0.5% of patients per year.AgeIn children, bioprostheses rapidly calcify and, therefore, undergo rapid degeneration and valve dysfunction. Incidence of bioprosthetic failure is much higher in patients younger than 40 years. The incidence of having any prosthetic valve complication decreases with age.
PreviousProceed to Clinical Presentation , Prosthetic Heart Valves





Is it true that newest laboratory equipment is capable to grow artificial tissues, for example, valves that may be used instead these, mentioned in your article?
ReplyDelete