Since its introduction in 1900, the emergency department thoracotomy (EDT) has been a subject of intense debate. It is a drastic, last-ditch effort to save the life of a patient in extremis due to chest injury.[1] Although some studies boast a 60% survival rate, others have argued that EDT is a futile and expensive procedure that only places health care providers at significant personal risk. Further, indications for EDT have widely varied. For these reasons, the EDT remains a controversial but potentially lifesaving procedure in a select group of patients.[2, 3]
The causes of acute circulatory arrest after chest injury include hemorrhagic shock due to injury to the heart or intrathoracic vasculature, cardiac tamponade, and tension pneumothorax.
The primary goals of EDT include the following[4] :
Hemorrhage controlRelease of cardiac tamponade[5, 6] Facilitation of internal/open cardiac massage[7, 8] Prevention of air embolismExposure of the descending thoracic aorta for cross-clampingRepair cardiac or pulmonary injuryEmergent thoracotomy typically takes place in the emergency department or operating room. It is crucial for the emergency provider to consult a surgeon upon the patient’s arrival to facilitate with the procedure if possible or to manage the patient subsequent to the thoracotomy. Emergent thoracotomies have been successfully performed in the prehospital setting by physicians and emergency medical service teams.[9, 10, 11]
NextIndicationsThe indications for EDT have been much debated.
To simplify the issue, the American College of Surgeons Committee on Trauma has instituted general guidelines on this subject.[12]
The decision to perform an EDT is determined by the presence of signs of life and the mechanism and location of injury.
Increased thoracotomy survival rates are associated with signs of life in the ED, including the following:
Pupillary responseSpontaneous ventilationPresence of carotid pulseMeasurable or palpable blood pressureExtremity movementCardiac electrical activityThoracic injuries (as opposed to abdominal injuries) can be identified and treated during EDT.
Survival for blunt injury is significantly lower than for penetrating injury due to conditions such as cardiac contusion, cardiac rupture, and aortic rupture.[13, 14, 15] Many consider an attempt to resuscitate a blunt trauma patient in cardiac arrest futile.[16]
Stab wounds (as opposed to gunshot wounds [GSW]) are associated with a higher success rate. GSW injuries are usually unable to spontaneously seal because of the large nature of the missile injury pattern.[1, 17]
The following are also associated with increased survival:
Higher blood pressureHigher respiratory ratesHigher Glasgow coma scale scoresAccepted indications for EDTPenetrating thoracic injury with the following conditions:
Previously witnessed cardiac activity (prehospital or in-hospital)Unresponsive hypotension (systolic blood pressure [SBP] [18]Blunt thoracic injury with the following conditions:
Previously witnessed cardiac activity (prehospital or in-hospital)Rapid exsanguination from the chest tube (>1,500 mL immediately returned)Unresponsive hypotension (SBPAmerican College of Surgeons Committee on Trauma indications for EDTÂ [19]
Precordial wound in a patient with prehospital cardiac arrestTrauma patient with cardiac arest after arrival to EDProfound hypotension (Relative indications for EDTPenetrating thoracic injury with traumatic arrest without previously witnessed cardiac activityPenetrating nonthoracic injury (eg, abdominal, peripheral) with traumatic arrest with previously witnessed cardiac activity (prehospital or in-hospital) Blunt thoracic injuries with traumatic arrest with previously witnessed cardiac activity (pre-hospital or in-hospital).The decision to perform an EDT should be made on a case-by-case basis due to exceptions and reported survivors who exceeded the above thresholds.[16, 20, 21]
PreviousNextContraindicationsEDT should not be performed in patients under the following conditions:
Blunt injury without witnessed cardiac activity (prehospital)[22, 23] Penetrating abdominal trauma without cardiac activity (prehospital)Nontraumatic arrestSevere head injurySevere multisystem injuryImproperly trained teamInsufficient equipmentA 2011 prospective multicenter study suggests that EDT does not yield survival if the following are noted[24] :
Blunt trauma with more than 10 minutes of prehospital cardiopulmonary resuscitation (CPR) without responsePenetrating trauma with more than 15 minutes of prehospital CPR without responseAsystole without cardiac tamponadeAs mentioned, the decision to perform EDT should be made on a case-by-case basis because the literature demonstrates rare survival even in patients with relatively favorable parameters.[16, 20, 21]
PreviousNextAnesthesiaMost patients undergoing EDT are comatose or medically sedated and/or paralyzed from airway management.The first consideration should be to intubate the patient for adequate control and comfort. If orotracheal intubation is not possible (eg, unsuccessful intubation or anticipated difficult intubation), adequate analgesic and amnestic agents are indicated. Ideally, agents that have minimal effects on the cardiovascular system should be used. For more information, see Procedural Sedation. PreviousNextEquipmentPersonal protective equipment and preparationGlovesSterile glovesGownFace shieldPovidone iodine (Betadine)Sterile drapesTo enter the chest cavity - Thoracotomy trayScalpel, No. 10 or No. 20 bladeMayo scissors (alternatively, Metzenbaum scissors)Rib spreaders (eg, Finochietto)Trauma shears or saw (eg, Gigli)To control hemorrhage and repair injuryTissue/tooth forcepsSatinsky vascular clamps (large and small)Long and short needle holders (eg, Hegar)Nonabsorbable sutures (silk), 2-0 or larger, on large round-body needleCardiovascular Ethibond sutures, 3-0Teflon pledgets plus polypropylene or large braided suturesSuture scissorsAortic clamp instrumentKelly clampSkin staplerHigh-volume suction deviceLaparotomy packsTonsil clampsFoley catheter, 20F with 30-mL balloonLaparotomy padsTeflon patchesInternal defibrillator (charge to 10 J to start)Chest tube, 30FACLS medicationsPreviousNextPositioningThe patient should be supine.Place several towels beneath the left scapula.Raise the patient’s left arm above the head. The patient’s arm may be secured in the elevated position with tape or restraints, if necessary. PreviousNextTechniquePreparationPrepare the patient’s left and right chest with iodine.Drape the area with sterile sheets or towels.Airway control is typically indicated for all patients and is best performed through standard orotracheal techniques. If exposure to the thoracic organs is impeded because of frequent lung inflation, selective right mainstem intubation may be performed by passing the endotrachial tube to 30 cm. A nasogastric tube may be passed to help differentiate the esophagus from the aorta. The procedure should not be delayed for passage of the nasogastric tube. In female patients, an assistant should retract the breast upward prior to incision.Anterolateral thoracotomy approachThe incision is typically made over the fifth rib into the fourth intercostal space, beginning at the sternum and extending to the posterior axillary line.
The incision should be deep enough to partially transect the latissimus dorsi muscle.Time should not be taken to count the rib spaces.In patients with a suspected left subclavian injury, the incision may be made in the third intercostal space.A left-sided approach is made in all traumatic arrests and in patients with left-sided chest injuries, as shown below. (A right-sided approach may be used in nonarrested patients with right-sided injuries.)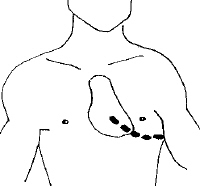 A skin incision is made above the fifth rib into the left fourth intercostal space from the sternal border to the midaxillary line. Separate the skin, subcutaneous fat, and superficial portions of the pectoralis and serratus muscles with a No. 20 scalpel blade. Stop ventilation momentarily just before entering the pleural cavity to allow the lung to collapse and minimize iatrogenic injury. Use a scalpel to make a small incision through the intercostal muscles.Place one blade of blunt-ended scissors into the hole; then, completely transect the intercostal muscles. The operator may insert the fourth and fifth fingers of his or her free hand into the intercostal space and gently push away the lung to prevent injury to it by the scissors. After transection of the intercostals muscles, place a rib spreader between the ribs to expose the intrathoracic contents. The rib spreader should be placed with the handle downward to permit for extension of the incision into the right chest if necessary. Upon visualization of the thoracic cavity, use suction to evacuate clots and blood.If injury to the right side of the heart is suspected, another incision can be made on the right, creating what is known as a clamshell (bilateral anterolateral thoracotomy). Alternatively, the sternum can be divided with trauma shears or a Gigli saw to extend the thoracotomy across the midline (called a trap door). Transection of the internal mammary arteries by this technique may result in significant bleeding once blood flow is restored. Pericardiotomy
A skin incision is made above the fifth rib into the left fourth intercostal space from the sternal border to the midaxillary line. Separate the skin, subcutaneous fat, and superficial portions of the pectoralis and serratus muscles with a No. 20 scalpel blade. Stop ventilation momentarily just before entering the pleural cavity to allow the lung to collapse and minimize iatrogenic injury. Use a scalpel to make a small incision through the intercostal muscles.Place one blade of blunt-ended scissors into the hole; then, completely transect the intercostal muscles. The operator may insert the fourth and fifth fingers of his or her free hand into the intercostal space and gently push away the lung to prevent injury to it by the scissors. After transection of the intercostals muscles, place a rib spreader between the ribs to expose the intrathoracic contents. The rib spreader should be placed with the handle downward to permit for extension of the incision into the right chest if necessary. Upon visualization of the thoracic cavity, use suction to evacuate clots and blood.If injury to the right side of the heart is suspected, another incision can be made on the right, creating what is known as a clamshell (bilateral anterolateral thoracotomy). Alternatively, the sternum can be divided with trauma shears or a Gigli saw to extend the thoracotomy across the midline (called a trap door). Transection of the internal mammary arteries by this technique may result in significant bleeding once blood flow is restored. PericardiotomyThis should be the second step if a tamponade is suspected. Otherwise, the aorta may be cross-clamped first (see below). If the visualized thoracic contents do not reveal any obvious injury but cardiac injury is suspected, the pericardium should be opened. Visual inspection of the pericardium is not sensitive to rule out cardiac tamponade, and the pericardium should always be opened to assess for retro cardiac blood.
Use tissue forceps to grasp the parietal pericardium and incise the pericardium with scissors.
Enter the pericardium anterior to the phrenic nerve and near the diaphragm to avoid injury to the great vessels.The phrenic nerve, often difficult to visualize in the ED, is a tendonlike structure. Upon incision of the pericardium, take care to keep the point of the scissors parallel to the heart to prevent damage to the myocardium when extending the incision. Alternatively, after the initial incision into the pericardium, the operator can use his or her fingers to tear the pericardium. Such blunt dissection helps to avoid laceration of the phrenic nerve. The heart should be delivered from the pericardial sack for inspection, as shown below.If cardiac lacerations are seen, digital occlusion, interrupted sutures, or clamps (Satinsky) can be used as indicated. (see Cardiac Repair below) Anatomy seen after a left-sided thoracotomy. (A) heart, (B) phrenic nerve, (C) cut and retracted pericardium, (D) diaphragm, and (E) lung. Aortic cross-clamping
Anatomy seen after a left-sided thoracotomy. (A) heart, (B) phrenic nerve, (C) cut and retracted pericardium, (D) diaphragm, and (E) lung. Aortic cross-clampingCross-clamping the descending aorta redistributes the available blood flow to the coronary and cerebral arteries.
Selective clamping of the descending aorta near the level of the diaphragm can also be used to control hemorrhage in abdominal vascular injuries.
Clamping distally is ideal because it maximizes spinal cord perfusion and because the aorta is relatively mobile at this location.
Retract the left lung superiorly to expose the aorta.Bluntly dissect the mediastinal pleura with a Kelly clamp to reveal the mediastinal structures. The aorta lies anterior to the vertebrae, whereas the esophagus lies anterior and medial to the aorta, as shown below. While the aorta is said to feel rubbery, firm, and pulsatile, a hypotensive aorta is often difficult to distinguish from the esophagus.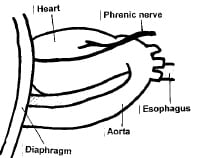 Lateral view of the anatomy encountered on left-sided thoracotomy. A nasogastric tube may be placed; palpation of this rigid tube is a way to differentiate the esophagus from the descending aorta. Occlusion of the aorta above the level of injury can be performed either through digital occlusion or with the use of an aortic tamponade instrument. Take care to not injure aortic or esophageal tissues. Organs that are distal to the aorta, including the bowel, kidneys, liver, and spinal cord, may become ischemic after occlusion.Clamp time should be limited to 30 minutes or less.However, one study found that patients who underwent cross-clamping of the aorta for up to 60 minutes in emergency thoracotomy had no significant decrease in organ function.
Lateral view of the anatomy encountered on left-sided thoracotomy. A nasogastric tube may be placed; palpation of this rigid tube is a way to differentiate the esophagus from the descending aorta. Occlusion of the aorta above the level of injury can be performed either through digital occlusion or with the use of an aortic tamponade instrument. Take care to not injure aortic or esophageal tissues. Organs that are distal to the aorta, including the bowel, kidneys, liver, and spinal cord, may become ischemic after occlusion.Clamp time should be limited to 30 minutes or less.However, one study found that patients who underwent cross-clamping of the aorta for up to 60 minutes in emergency thoracotomy had no significant decrease in organ function. Avoid cross-clamping the aorta in normotensive patients because the elevated afterload compromises cardiac circulation.[25]
Cardiac repairLarge wounds to the heart may be repaired with pledgetted sutures, incomplete mattress sutures, horizontal mattress sutures, or continuous running sutures. Nonabsorbable sutures, such as polypropylene or nylon, and even staple guns may be used.[26] The coronary arteries must not be compromised during repair; this is usually accomplished with mattress sutures. Cardiac exsanguination may be temporized by placing a Foley catheter inside the wound, inflating the catheter balloon, and then withdrawing the catheter to occlude the defect. Clamp the catheter to prevent exsanguination. Digital occlusion may also be used to stop bleeding temporarily.If multiple cardiac or great vessel gunshot wounds are seen on EDT, resuscitative efforts may be terminated because of limited surival probablility.[27] Internal cardiac massage/open chest CPRNo scientific consensus has been reached on the use of this procedure[16] . Perform internal cardiac massage with a 2-handed technique to avoid perforation of the ventricle with your thumb.Compared with standard CPR, which delivers up to 20% of the cardiac output, internal CPR produces up to 55% of the body's baseline perfusion. Open-chest CPR has been shown to improve coronary perfusion pressure and increases return of spontaneous circulation with equal benefit in penetrating and blunt trauma.[28, 29, 30] Continue this resuscitation effort for 20 minutes before termination.[16] Other considerationsInternal defibrillation begins at 20 joules and increases to 40-50 joules. Avoid touching the coronary arteries with the paddles.Fluid resuscitation should begin after hemorrhage control. Warmed fluids, blood, and clotting factors are likely necessary.Inotropic support may be required after adequate fluid resuscitation in cases of cardiogenic shock.Bleeding vasculature may be temporized with atraumatic clamps or sutures and emergently repaired by a specialist.The pulmonary hilum may be cross-camped in cases of major pulmonary hemorrhage.PreviousNextPearlsSurvival after EDT in blunt trauma patients is much lower than with penetrating injury.[31] Some recommend not performing EDT in patients with blunt trauma, owing to the particularly low survival rates.[3, 15, 17, 32, 33, 34] Control of the airway via standard orotracheal intubation technique is strongly advised prior to performing EDT. Selective intubation of the right mainstem bronchus is the preferred method. This allows for both ventilation and oxygenation of the patient via the right lung as well as decreased risk of injury to the left lung via decreased left lung expansion during a left-sided anterolateral thoracotomy. To intubate the right mainstem bronchus, directly visualize the vocal cords to pass the endotracheal (ET) tube into the trachea, and then blindly pass the ET tube to approximately 30 cm. Either prior to EDT or while the procedure is being performed, an assistant should pass a nasogastric tube to help distinguish the esophagus from the aorta upon exploration of the thoracic contents. Immediately obtain a surgical consult. If the patient survives the EDT, they need to be taken expediently to the operating room. Use the left anterolateral thoracotomy approach when the site of the injury is unknown and the patient’s status requires immediate intervention for possible intrathoracic injuries. Incision over the fifth rib with dissection into the fourth intercostal space provides the best access to the heart and great vessels. This incision is just beneath the nipple in men or along the inframammary fold in women. The rib spreaders should be placed with the handle downward to permit for extension of the incision into the right chest if necessary. Avoid making the incision too low. The location of the heart is commonly thought of as lower than it actually is.The incision should be made just above the rib to avoid injury to the intercostals neurovascular bundle.Gaining access to the thoracic cavity should take no longer than 1-2 minutes.When the patients clinical status allows, urgent rather than emergent thoracotomy can be performed to minimize the dangers incumbent to this procedure in the ED.[35] Large amounts of blood products are used in the resuscitation of patients undergoing EDT.Consider potential organ donor rescue after EDT arrest.[36] PreviousNextComplicationsEDT is a potentially lifesaving procedure; however, its complications must be weighed against its benefits.
Specific complications of EDT include the following:
Neurologic complications from hypoperfusion: Anoxic brain death occurs in as many as 50% of survivors, requiring ongoing institutional care.[37] Recurrent bleeding from chest wall or internal mammary arteryDamage to the coronary arteriesOther cardiac damage resulting in ventricular septal defects, aortic valvular irregularities, atrial septal defects, and cardiac conduction defects Damage to the esophagus during aortic cross-clampingDamage to the phrenic nerveIschemia to distal organs and spinal cord due to cross-clamping of aortaThe potential for transmission of blood-borne pathogens from the patient to the clinicians performing the procedure is also a very real risk. The seroprevalence of the human immunodeficiency virus (HIV) in urban EDs in the United States has been reported to range from 1.4-19%.[38, 39, 40]
Previous Contributor Information and DisclosuresAuthorGretchen S Lent, MD Attending Physician, Department of Emergency Medicine, Torrance Memorial Medical Center
Disclosure: Nothing to disclose.
Neel Kumar, MD Staff Physician, Department of Emergency Medicine, The Permanente Medical Group, Sacramento Medical Center
Disclosure: Pfizer Stockholder None
Luis M Lovato, MD Associate Clinical Professor, University of California, Los Angeles, David Geffen School of Medicine; Director of Critical Care, Department of Emergency Medicine, Olive View-UCLA Medical Center
Luis M Lovato, MD is a member of the following medical societies: Alpha Omega Alpha, American College of Emergency Physicians, and Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Mary L Windle, PharmD Adjunct Associate Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Nothing to disclose.
Brett C Sheridan, MD, FACS Associate Professor of Surgery, University of North Carolina at Chapel Hill School of Medicine
Disclosure: Nothing to disclose.
The authors and editors of Medscape Reference gratefully acknowledge the assistance of Lars Grimm with the literature review and referencing for this article.
ReferencesSiram, Suryanarayana, Oyetunji T, Johnson SM, Khoury, AL, et al. Predictors for survival of penetrating trauma using emergency department thoracotomy in an urban trauma center: the Cardiac Instability Score. Journal of the National Medical Association. Feb 2010;102(2):126-130. [Medline].
Branney SW, Moore EE, Feldhaus KM, Wolfe RE. Critical analysis of two decades of experience with postinjury emergency department thoracotomy in a regional trauma center. J Trauma. Jul 1998;45(1):87-94; discussion 94-5. [Medline].
Hunt PA, Greaves I, Owens WA. Emergency thoracotomy in thoracic trauma-a review. Injury. Jan 2006;37(1):1-19. [Medline].
Kirkpatrick AW, Ball CG, D'Amours SK, Zygun D. Acute resuscitation of the unstable adult trauma patient: bedside diagnosis and therapy. Can J Surg. Feb 2008;51(1):57-69. [Medline].
Menaker J, Cushman J, Vermillion JM, Rosenthal RE, Scalea TM. Ultrasound-diagnosed cardiac tamponade after blunt abdominal trauma-treated with emergent thoracotomy. J Emerg Med. Jan 2007;32(1):99-103. [Medline].
Leidel BA, Kanz KG, Kirchhoff C, Bürklein D, Wismüller A, Mutschler W. [Cardiac arrest following blunt chest injury. Emergency thoracotomy without ifs or buts?]. Unfallchirurg. Oct 2007;110(10):884-90. [Medline].
Boczar ME, Howard MA, Rivers EP, Martin GB, Horst HM, Lewandowski C. A technique revisited: hemodynamic comparison of closed- and open-chest cardiac massage during human cardiopulmonary resuscitation. Crit Care Med. Mar 1995;23(3):498-503. [Medline].
Jackson RE, Freeman SB. Hemodynamics of cardiac massage. Emerg Med Clin North Am. Dec 1983;1(3):501-13. [Medline].
Keogh SP, Wilson AW. Survival following pre-hospital arrest with on-scene thoracotomy for a stabbed heart. Injury. Sep 1996;27(7):525-7. [Medline].
Davies GE, Lockey DJ. Thirteen survivors of prehospital thoracotomy for penetrating trauma: a prehospital physician-performed resuscitation procedure that can yield good results. J Trauma. May 2011;70(5):E75-8. [Medline].
Coats TJ, Keogh S, Clark H, Neal M. Prehospital resuscitative thoracotomy for cardiac arrest after penetrating trauma: rationale and case series. J Trauma. Apr 2001;50(4):670-3. [Medline].
Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons-Committee on Trauma. Practice management guidelines for emergency department thoracotomy. J Am Coll Surg. Sep 2001;193(3):303-9. [Medline].
Velmahos GC, Degiannis E, Souter I, Allwood AC, Saadia R. Outcome of a strict policy on emergency department thoracotomies. Arch Surg. Jul 1995;130(7):774-7. [Medline].
Feliciano DV, Bitondo CG, Cruse PA, Mattox KL, Burch JM, Beall AC Jr. Liberal use of emergency center thoracotomy. Am J Surg. Dec 1986;152(6):654-9. [Medline].
Ivatury RR, Kazigo J, Rohman M, Gaudino J, Simon R, Stahl WM. "Directed" emergency room thoracotomy: a prognostic prerequisite for survival. J Trauma. Aug 1991;31(8):1076-81; discussion 1081-2. [Medline].
Moriwaki Y, Sugiyama M, Yamamoto T, Tahara Y, Toyoda H, Kosuge T, et al. Outcomes from prehospital cardiac arrestin blunt trauma patients. World Journal of Surgery. Jan 2011;35:34-45. [Medline].
Rhee PM, Acosta J, Bridgeman A, Wang D, Jordan M, Rich N. Survival after emergency department thoracotomy: review of published data from the past 25 years. J Am Coll Surg. Mar 2000;190(3):288-98. [Medline].
Iwata T, Inoue K, Hige M, Yamazaki K, Kawata Y, Suehiro S. Multiple thoracoabdominal gunshot wounds with complicated trajectories. Jpn J Thorac Cardiovasc Surg. Oct 2006;54(10):444-7. [Medline].
American College of Surgeons Committee on Trauma. Advanced trauma life support. 7th ed. Chicago, Ill: American College of Surgeons Committee on Trauma; 2004.
Pickens JJ, Copass MK, Bulger EM. Trauma patients receiving CPR: predictors of survival. J Trauma. 2005;5:951-958.
Seamon MJ, Fischer CA, Gaughan JP, Kulp H, Dempsey DT, Goldberg AJ. Emergency department thoracotomy: survivial of the least expected. World J Surg. 2008;32:604-612.
Cogbill TH, Moore EE, Millikan JS, Cleveland HC. Rationale for selective application of Emergency Department thoracotomy in trauma. J Trauma. Jun 1983;23(6):453-60. [Medline].
Kavolius J, Golocovsky M, Champion HR. Predictors of outcome in patients who have sustained trauma and who undergo emergency thoracotomy. Arch Surg. Oct 1993;128(10):1158-62. [Medline].
Moore EE, Knudson MM, Burlew CC, Inaba K, Dicker RA, Biffl WL, et al. Defining the limits of resuscitative emergency department thoracotomy: a contemporary Western Trauma Association perspective. Journal of Trauma-Injury Infection and Critical Care. Feb 2011;70(2):334-339. [Medline].
Garcia-Rinaldi R, Defore WW, Mattox KL, Beall AC Jr. Unimpaired renal, myocardial and neurologic function after cross clamping of the thoracic aorta. Surg Gynecol Obstet. Aug 1976;143(2):249-52. [Medline].
Macho JR, Markison RE, Schecter WP. Cardiac stapling in the management of penetrating injuries of the heart: rapid control of hemorrhage and decreased risk of personal contamination. J Trauma. May 1993;34(5):711-5; discussion 715-6. [Medline].
Seamon MJ, Shiroff AM, Franco M, Stawicki SP, Molina EJ, Gaughan JP, et al. Emergency department thoracotomy for penetrating injuries of the heart and great vessels: an appraisal of 283 consecutive cases from two urban trauma centers. Journal of Trauma-Injury Infection and Critial Care. Dec 2009;67(6):1257-1258. [Medline].
Boczar ME, Howard MA, Rivers EP. A technique revisited: hemodynamic comparison of closed and open-chest cardiac massage during human cardiopulmonary resuscitation. Crit Care Med. 1995;23:498-503.
Takino M, Okada Y. The optimum timing of resuscitative thoracotomy for non-traumatic out-of-hospital cardiac arrest. Resuscitation. 1993;26:69-74.
Weil MH, Rackow EC, Trevino R. Difference in acid-base state between venous and arterial blood during cardiopulmonary resuscitation. N Engl J Med. 1986;315:153-156.
Hoth JJ, Scott MJ, Bullock TK, Stassen NA, Franklin GA, Richardson JD. Thoracotomy for blunt trauma: traditional indications may not apply. Am Surg. Dec 2003;69(12):1108-11. [Medline].
Lustenberger T, Labler L, Stover JF, Keel MJ. Resuscitative emergency thoracotomy in a Swiss trauma centre. Br J Surg. Apr 2012;99(4):541-8. [Medline].
Hopson LR, Hirsh E, Delgado J, et al. Guidelines for withholding or termination of resuscitation in prehospital traumatic cardiopulmonary arrest. J Am Coll Surg. Mar 2003;196(3):475-81. [Medline].
Powell DW, Moore EE, Cothren CC, et al. Is emergency department resuscitative thoracotomy futile care for the critically injured patient requiring prehospital cardiopulmonary resuscitation?. J Am Coll Surg. Aug 2004;199(2):211-5. [Medline].
Kremer H, Wilson J. Penetrating cardiac injury with urgent not emergent thoracotomy. Missouri Medicine. Sept-Oct2010;107(5):328-330. [Medline].
Schnuriger B, Inaba K, Branco BC, Salim A, Russell K, Lam L, et al. Organ donation: an important outcome after resuscitative thoracotomy. Journal of the American College of Surgeons. Oct 2010;211(4):450-455.
Connery C, Geller E, Dulchavsky S, Kreis DJ Jr. Paraparesis following emergency room thoracotomy: case report. J Trauma. Mar 1990;30(3):362-3. [Medline].
Baker JL, Kelen GD, Sivertson KT, Quinn TC. Unsuspected human immunodeficiency virus in critically ill emergency patients. JAMA. May 15 1987;257(19):2609-11. [Medline].
Kelen GD, Fritz S, Qaquish B, Floccare D, DiGiovanna T, Baker JL. Substantial increase in human immunodeficiency virus (HIV-1) infection in critically ill emergency patients: 1986 and 1987 compared. Ann Emerg Med. Apr 1989;18(4):378-82. [Medline].
Soderstrom CA, Furth PA, Glasser D, Dunning RW, Groseclose SL, Cowley RA. HIV infection rates in a trauma center treating predominantly rural blunt trauma victims. J Trauma. Nov 1989;29(11):1526-30. [Medline].
Edens JW, Beekley AC, Chung KK, Cox ED, Eastridge BJ, Holcomb JB, et al. Longterm outcomes after combat casualty emergency department thoracotomy. J Am Coll Surg. Aug 2009;209(2):188-97. [Medline].
Morrison JJ, Mellor A, Midwinter M, Mahoney PF, Clasper JC. Is pre-hospital thoracotomy necessary in the military environment?. Injury. May 2011;42(5):469-73. [Medline].
Roberts JR, Hedges JR, eds. Clinical Procedures in Emergency Medicine. 4th ed. Philadelphia, Pa: WB Saunders; 2004.
Seamon MJ, Goldberg AJ, Schwab CW. Emergency department thoracotomy for gunshot wounds of the heart and great vessels. J Trauma. Jun 2010;68(6):1514-5. [Medline].
Â
 A skin incision is made above the fifth rib into the left fourth intercostal space from the sternal border to the midaxillary line. Anatomy seen after a left-sided thoracotomy. (A) heart, (B) phrenic nerve, (C) cut and retracted pericardium, (D) diaphragm, and (E) lung. Lateral view of the anatomy encountered on left-sided thoracotomy.
A skin incision is made above the fifth rib into the left fourth intercostal space from the sternal border to the midaxillary line. Anatomy seen after a left-sided thoracotomy. (A) heart, (B) phrenic nerve, (C) cut and retracted pericardium, (D) diaphragm, and (E) lung. Lateral view of the anatomy encountered on left-sided thoracotomy. 
  View Table List Read more about Emergency Bedside Thoracotomy on MedscapeRelated News and Articles
 View Table List Read more about Emergency Bedside Thoracotomy on MedscapeRelated News and ArticlesA Lost Art?
Bedside Ultrasound and the Assessment of Renal Colic
Bedside Echo Could Facilitate ER Diagnosis of Pulmonary Embolism
Medscape Reference © 2011 WebMD, LLC, Emergency Bedside Thoracotomy






0 comments:
Post a Comment