Atrial tachycardia is a supraventricular tachycardia (SVT) that does not require the atrioventricular (AV) junction, accessory pathways, or ventricular tissue for its initiation and maintenance. It occurs in persons with normal hearts and in those with structurally abnormal hearts, including individuals with congenital heart disease (particularly after surgery for repair or correction of congenital or valvular heart disease).
In patients with structurally normal hearts, atrial tachycardia is associated with a low mortality rate. Patients with underlying structural heart disease, congenital heart disease, or lung disease are less likely to be able to tolerate this rhythm disturbance.
Essential updates: Distinguishing between left- and right-sided atrial tachycardiaPatterns derived from combining pulmonary artery, right atrial, and coronary sinus potentials can be used to distinguish between left- and right-sided atrial tachycardia, according to a study by Hirai et al. Using sequences obtained using electrode and ablation catheters, the investigators were able to predict the presence of left-sided atrial tachycardia with 90% accuracy, as well as a sensitivity and specificity of 78% and 100%, respectively.[1]
Signs and symptomsManifestations of atrial tachycardia include the following:
Rapid pulse rate: In most atrial tachycardias, the rapid pulse is regular; it may be irregular in rapid atrial tachycardias with variable AV conduction and in multifocal atrial tachycardia (MAT) Episodic or paroxysmal occurrenceSudden onset of palpitationsContinuous, sustained, or repetitive tachycardia: If atrial tachycardia is due to enhanced automaticityWarm-up phenomenon: Tachycardia gradually speeds up soon after onset (may be clinically inapparent)Dyspnea, dizziness, lightheadedness, fatigue, or chest pressure: In tachycardic episodes accompanied by palpitationsSyncope: With rapid rate and severe hypotensionHeart-failure symptoms and reduced effort tolerance: Early manifestations of tachycardia-induced cardiomyopathy in patients with frequent or incessant tachycardiaIn patients with MAT, the history may disclose an underlying illness that is causing the tachycardia. Such illnesses include pulmonary, cardiac, metabolic, and endocrinopathic disorders. Chronic obstructive pulmonary disease (COPD) is the most common underlying disease process (60%) in MAT.
Reentrant atrial tachycardia is not uncommon in patients with a history of a surgically repaired atrial septal defect. The scar tissue in the atrium may give rise to the formation of a reentrant circuit.
On physical examination, the primary abnormal finding is a rapid pulse rate. The rate is usually regular, but it may be irregular in rapid atrial tachycardias with variable AV conduction and in MAT. Blood pressure may be low in patients presenting with fatigue, lightheadedness, or presyncope.
See Clinical Presentation for more detail.
DiagnosisWorkup for atrial tachycardia can employ the following diagnostic tools:
12-lead electrocardiography: To help identify, locate, and differentiate atrial tachycardiaHolter monitoring: To analyze the onset and termination of atrial tachycardia, identify the AV conduction block during the episode, and correlate the symptoms to atrial tachycardia Endocardial mapping: To localize atrial tachycardiaThe following laboratory studies may be indicated to exclude systemic causes of sinus tachycardia:
Serum chemistry: To exclude electrolyte disordersBlood hemoglobin level and red blood cell (RBC) counts: To seek evidence of anemiaArterial blood gas level: To define pulmonary statusSerum digoxin assay: When digitalis intoxication is suspectedThe following imaging studies can be useful in the evaluation of patients with atrial tachycardia:
Chest radiography: In patients with tachycardia-induced cardiomyopathy or complex congenital heart diseaseComputed tomography (CT) scanning: To exclude pulmonary embolism, assess the anatomy of pulmonary veins, and provide images prior to ablative procedure Echocardiography: To rule out structural heart disease and assess left atrial size, pulmonary arterial pressure, left ventricular function, and pericardial pathologySee Workup for more detail.
ManagementThe primary treatment during a bout of atrial tachycardia is considered to be rate control using AV nodal blocking agents (eg, beta blockers, calcium channel blockers). Antiarrhythmic drugs can prevent recurrences and may be required; a calcium channel blocker or beta blocker also may be required in combination therapy. Specific antiarrhythmic therapies include the following:
Atrial tachycardia from triggered activity: Verapamil, beta blockers, and adenosineAtrial tachycardia from enhanced automaticity: Beta blockers, but overall success rates are lowRefractory recurrent atrial tachycardia: Class Ic antiarrhythmic drugsMaintenance of sinus rhythm: Class III antiarrhythmic drugsNonpharmacologic therapies for atrial tachycardia include the following:
Cardioversion: For patients in whom the rhythm is not well-tolerated hemodynamically and in whom rate-control drugs are ineffective or contraindicated Radiofrequency catheter ablation: For symptomatic, medically refractory patients[2, 3] Surgical ablation: For patients with complex congenital heart diseaseMultifocal atrial tachycardia
Treatment of MAT involves treatment and/or reversal of the precipitating cause. Therapy also may include the following:
Calcium channel blockers: Used as the first line of treatmentMagnesium sulfate: When administered to correct hypokalemia, most patients convert to normal sinus rhythm (NSR)Beta blockersAntiarrhythmicsIn very rare cases, when MAT is persistent and refractory, AV junctional radiofrequency ablation and permanent pacemaker implantation should be considered. Such treatment can provide symptomatic and hemodynamic improvement and prevent the development of tachycardia-mediated cardiomyopathy.[4]
See Treatment and Medication for more detail.
Image Library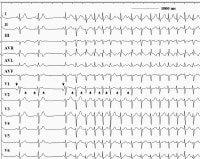 This 12-lead electrocardiogram demonstrates an atrial tachycardia at a rate of approximately 150 beats per minute. Note that the negative P waves in leads III and aVF (upright arrows) are different from the sinus beats (downward arrows). The RP interval exceeds the PR interval during the tachycardia. Note also that the tachycardia persists despite the atrioventricular block. NextBackground
This 12-lead electrocardiogram demonstrates an atrial tachycardia at a rate of approximately 150 beats per minute. Note that the negative P waves in leads III and aVF (upright arrows) are different from the sinus beats (downward arrows). The RP interval exceeds the PR interval during the tachycardia. Note also that the tachycardia persists despite the atrioventricular block. NextBackgroundAtrial tachycardia is defined as a supraventricular tachycardia (SVT) that does not require the atrioventricular (AV) junction, accessory pathways, or ventricular tissue for its initiation and maintenance. Atrial tachycardia can be observed in persons with normal hearts and in those with structurally abnormal hearts, including those with congenital heart disease and particularly after surgery for repair or correction of congenital or valvular heart disease.
In adults, tachycardia is usually defined as a heart rate more than 100 beats per minute (bpm). In children, the definition of tachycardia varies because the normal heart rate is age dependent, as follows:[5, 6]
Age 1-2 days: 123-159 bpmAge 3-6 days: 129-166 bpmAge 1-3 weeks: 107-182 bpmAge 1-2 months: 121-179 bpmAge 3-5 months: 106-186 bpmAge 6-11 months: 109-169 bpmAge 1-2 years: 89-151 bpmAge 3-4 years: 73-137 bpmAge 5-7 years: 65-133 bpmAge 8-11 years: 62-130 bpmAge 12-15 years: 60-119 bpmAs in most SVTs, the electrocardiogram (ECG) typically shows a narrow QRS complex tachycardia (unless bundle branch block aberration occurs). Heart rates are highly variable, with a range of 100-250 bpm. The atrial rhythm is usually regular. (See the image below.)
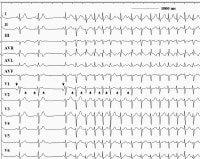 This 12-lead electrocardiogram demonstrates an atrial tachycardia at a rate of approximately 150 beats per minute. Note that the negative P waves in leads III and aVF (upright arrows) are different from the sinus beats (downward arrows). The RP interval exceeds the PR interval during the tachycardia. Note also that the tachycardia persists despite the atrioventricular block.
This 12-lead electrocardiogram demonstrates an atrial tachycardia at a rate of approximately 150 beats per minute. Note that the negative P waves in leads III and aVF (upright arrows) are different from the sinus beats (downward arrows). The RP interval exceeds the PR interval during the tachycardia. Note also that the tachycardia persists despite the atrioventricular block. The conducted ventricular rhythm is also usually regular. It may become irregular, however, especially at higher atrial rates, because of variable conduction through the AV node, thus producing conduction patterns such as 2:1, 4:1, a combination of those, or Wenckebach AV block.
The P wave morphology on the ECG may give clues to the site of origin and mechanism of the atrial tachycardia. In the case of a focal tachycardia, the P wave morphology and axis depend on the location in the atrium from which the tachycardia originates. In the case of macroreentrant circuits, the P wave morphology and axis depend on activation patterns (see Workup).
Multifocal atrial tachycardia (MAT) is an arrhythmia with an irregular atrial rate greater than 100 bpm. Atrial activity is well organized, with at least 3 morphologically distinct P waves, irregular P-P intervals, and an isoelectric baseline between the P waves.[7] Multifocal atrial tachycardia has previously been described by names such as chaotic atrial rhythm or tachycardia, chaotic atrial mechanism, and repetitive paroxysmal MAT. Go to Multifocal Atrial Tachycardia for more complete information on this topic.
Classification methodsA number of methods are used to classify atrial tachycardia. Classification in terms of origin can be based on endocardial activation mapping data, pathophysiologic mechanisms, and anatomy.
On the basis of endocardial activation, atrial tachycardia may be divided into the following 2 groups (see Presentation):
Focal atrial tachycardia: Arises from a localized area in the atria such as the crista terminalis, pulmonary veins, ostium of the coronary sinus, or intra-atrial septum. Reentrant atrial tachycardias: Usually macroreentrant; reentrant atrial tachycardias most commonly occur in persons with either structural or complex heart disease, particularly after surgery involving atrial incisions or scarring Other methods of classification are as follows:Pathophysiologic mechanisms: Atrial tachycardia can be classified as the result of enhanced automaticity, triggered activity, or reentry (see Pathophysiology) Anatomy: Classification of atrial tachycardia can be based on the location of the arrhythmogenic focus (see Anatomy)Diagnosis and treatmentA 12-lead ECG is an important tool to help identify, locate, and differentiate atrial tachycardia. Laboratory studies may be indicated to exclude systemic disorders that may be causing the tachycardia. Electrophysiologic study may be required. (See Workup.)
The primary treatment during a bout of atrial tachycardia is considered to be rate control using AV nodal blocking agents, such as beta blockers or calcium channel blockers (see Treatment and Medication). Cardioversion should be considered for any patient in whom the rhythm is not tolerated well hemodynamically and in whom rate control drugs are ineffective or contraindicated.
Radiofrequency catheter ablation for atrial tachycardia has become a highly successful and effective treatment option for symptomatic patients whose condition is refractory to medical therapy or who do not desire long-term antiarrhythmic therapy. It can cure macroreentrant and focal forms of atrial tachycardia. (See Treatment.)[8, 9]
PreviousNextAnatomyAtrial tachycardia can have a right or left atrial origin. Some atrial tachycardias actually originate outside the usual anatomic boundaries of the atria, in areas such as the superior vena cava, pulmonary veins, and vein of Marshall, where fingers of atrial myocardium extend into these locations. Rare locations, such as the noncoronary aortic cusp[2] and hepatic veins, have been described, as well. (See the video below.)
Propagation map of right atrial tachycardia originating from the right atrial appendage obtained with non-contact mapping using EnSite mapping system.A number of aspects of the atrial anatomy can contribute to the substrate for arrhythmia. The orifices of the vena cava, pulmonary veins, coronary sinus, atrial septum, and mitral and tricuspid annuli are potential anatomic boundaries for reentrant circuits.
Anisotropic conduction in the atria due to complex fiber orientation may create the zone of slow conduction. Certain atrial tissues, such as the crista terminalis and pulmonary veins, are common sites for automaticity or triggered activity. Additionally, disease processes or age-related degeneration of the atria may give rise to the arrhythmogenic substrate.
Abnormalities that have been reported at the sites of atrial tachycardia origin include the following[1] :
Extensive myocardial fibrosisMyocyte hypertrophyEndocardial fibrosisMononuclear cell infiltrationMesenchymal cell proliferationIslets of fatty tissueThinningBlebs PreviousNext, Atrial Tachycardia





0 comments:
Post a Comment