Primary pulmonary hypertension (PPH) is a rare disease characterized by elevated pulmonary artery pressure with no apparent cause. PPH is also termed precapillary pulmonary hypertension or, as is currently preferred, idiopathic pulmonary arterial hypertension (IPAH). Untreated IPAH leads to right-sided heart failure and death.
Essential update: FDA approves riociguat for pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertensionIn October 2013, the FDA approved riociguat (Adempas) for the treatment of pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension (CTEPH). Approval was based on 2 randomized, double-blind, placebo-controlled studies. A vasodilator that restores the nitric-oxide–soluble guanylate cyclase-cyclic guanosine monophosphate pathway, riociguat is approved for adults only; its safety in pediatric patients has not been determined.[1, 2]
Signs and symptomsCommon symptoms of IPAH include the following:
DyspneaWeaknessRecurrent syncopeCardiovascular examination in patients with pulmonary arterial hypertension (PAH) often reveals the following findings:
The pulmonic component of the second heart sound is usually increased, which may demonstrate fixed or paradoxic splitting in the presence of severe right ventricular dysfunction; occasionally, the second heart sound may be palpable Pulmonic regurgitation (Graham Steell murmur) may be apparentA murmur of tricuspid regurgitation can be present, and a right ventricular lift (heave) may be notedJugular venous pulsations may be elevated in the presence of volume overload, right ventricular failure, or both; large V waves are often present because of the commonly present severe tricuspid regurgitationOther findings may include the following:
Hepatomegaly with palpable pulsations of the liverAbnormal abdominal-jugular reflexAscites - Not uncommon in untreated patients and in patients with worsening decompensated right heart failurePitting edema - In the extremitiesPresacral edema - In patients who are bedriddenSee Clinical Presentation for more detail.
DiagnosisCardiac catheterization
Cardiac catheterization is the criterion standard test to definitively confirm any form of PAH. Excluding left-sided heart disease, including diastolic dysfunction, is especially important in these patients because of major treatment implications. Catheterization is also performed to determine pulmonary vasoreactivity, which may have implications in the initiation and titration of high-dose calcium channel blocker (CCB) therapy.
Laboratory studies
Antinuclear antibodyThyrotropinB-type natriuretic peptideImaging studies
RadiographyEchocardiographyComputed tomography (CT) and lung scanningPulmonary angiographyElectrocardiography
Electrocardiographic results are often abnormal in patients with PAH, revealing right atrial enlargement, right axis deviation, right ventricular hypertrophy, and characteristic ST depression and T-wave inversions in the anterior leads. However, some patients with IPAH have few or no abnormal electrocardiographic findings.
Histology
Several histologic subtypes are associated with pulmonary arteriopathy in IPAH, one of which involves in situ thrombosis.
Exercise testing
In patients with IPAH, values for peak exercise oxygen consumption, oxygen pulse, and ventilator equivalents (ratio of expired volume to carbon dioxide output [ie, wasted ventilation fraction] at the anaerobic threshold) during exercise are abnormal to varying degrees.
See Workup for more detail.
ManagementCalcium channel blocker therapy
Long-term treatment improves the quality of life and survival rate in patients who are proven responders to calcium channel blockers (CCBs). In general, CCBs are used at high doses in patients with IPAH.
Vasodilator therapy
For patients with IPAH in whom CCBs are contraindicated, ineffective, or poorly tolerated, guidelines from the American College of Chest Physicians (ACCP) recommend using the patient’s New York Heart Association (NYHA) functional class to guide the choice of vasodilator therapy.[3, 4] Grade A recommendations for vasodilator therapy by functional class from the ACCP are as follows:
Functional class II - SildenafilFunctional class III - Endothelin-receptor antagonists (bosentan), sildenafil, intravenous (IV) epoprostenol, or inhaled iloprostFunctional class IV - IV epoprostenol (treatment of choice)Transplantation and septostomy
Lung transplantation - A single- or double-lung transplant is indicated for patients who do not respond to medical therapySeptostomy - Atrial septostomy is a palliative procedure that may afford some benefit to patients whose condition is deterioratingSee Treatment and Medication for more detail.
Image library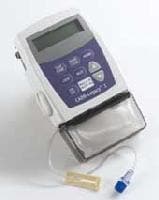 CADD Legacy ambulatory infusion pump. Courtesy SIMS Deltec, St. Paul, Minn. NextBackground
CADD Legacy ambulatory infusion pump. Courtesy SIMS Deltec, St. Paul, Minn. NextBackgroundPrimary pulmonary hypertension (PPH) is a rare disease characterized by elevated pulmonary artery pressure with no apparent cause. PPH is also termed precapillary pulmonary hypertension or, more recently, idiopathic pulmonary arterial hypertension (IPAH). The term IPAH is now the preferred term for pulmonary arterial hypertension of unknown etiology; thus, IPAH represents pulmonary vascular disease with a spectrum of clinical presentations.
Dresdale and colleagues first reported a hemodynamic account of IPAH in 1951.[5] However, the pathophysiology of IPAH remains poorly understood. At least 15-20% of patients previously thought to have IPAH actually have a familial form of PAH involving at least one genetic defect, which has only recently been characterized (see Pathophysiology).
Cardiac catheterization is the criterion standard test to definitively confirm any form of PAH, including IPAH. However, a thorough workup includes a range of tests to exclude all reasonable causes of secondary pulmonary hypertension (see Workup).
Until recently, calcium channel blockers (CCBs) had been the most widely used class of drugs for IPAH. Patients with IPAH in whom CCBs are contraindicated, ineffective, or poorly tolerated may respond to long-term vasodilator therapy (see Treatment and Management).
Treating IPAH requires significant knowledge of and exposure to the available therapies for IPAH and their potential complications. Because IPAH is relatively rare, management is best left to expert personnel at centers with regular exposure to these patients (see Treatment and Management).
Patient educationPatient education about this rare fatal disease is paramount. If applicable, instruct patients on how to administer their daily parenteral medication. For patient education information, see the Lung and Airway Center and Heart and Blood Vessels Center.
For more information, see the Medscape Reference article Pediatric Primary Pulmonary Hypertension.
PreviousNextPathophysiologyThe pathophysiology of IPAH is poorly understood. An insult (eg, hormonal, mechanical, other) to the endothelium may occur, possibly in the setting of increased susceptibility to pulmonary vascular injury (ie, multiple hit theory), resulting in a cascade of events characterized by vascular scarring, endothelial dysfunction, and intimal and medial (smooth muscle) proliferation.
At least 15-20% of patients previously thought to have IPAH actually have a familial form of PAH involving at least one genetic defect, which has only recently been characterized. The most common genetic defect in these cases involves the BMPR-II gene. However, only about a third of affected patients with a family history of PAH have an identifiable BMPR-II mutation. This suggests that additional genetic abnormalities and/or additional external factors may exist that predispose individuals to developing PAH.
In 2013, 6 mutations that appear to be associated with pulmonary arterial hypertension (PAH) and that may be treatable were discovered in a gene, KCNK3, that had not previously been linked to the disease. Each of the 6 mutations was linked to a loss of function of potassium ion channels.[6, 7] In vitro examination of the investigational agent ONO-RS-082 (2-[p-amylcinnamoyl]amino-4-chlorobenzoic acid), a phospholipase A2 inhibitor, found that for 2 of the 3 mutations tested, the drug restored function to nonworking potassium ion channels.
Early in PAH, as the pulmonary artery pressure increases because of increasing right ventricle work, thrombotic pulmonary arteriopathy occurs. Thrombotic pulmonary arteriopathy is characterized by in situ thrombosis of small muscular arteries. In later stages, as the pulmonary pressure continues to rise, plexogenic pulmonary arteriopathy develops. This is characterized by a remodeling of the pulmonary vasculature with intimal fibrosis and replacement of normal endothelial structure.
For more information, see the Medscape Reference article Persistent Newborn Pulmonary Hypertension.
Associated conditionsPulmonary vascular disease can be associated with portal hypertension (sometimes called portopulmonary hypertension), suggesting that patients with shunting of splanchnic blood, with or without liver disease, have a higher risk of developing PAH.
Additionally, exposure of the pulmonary circulation to substances from the splanchnic circulation that are normally detoxified via the liver may contribute to the development of pulmonary hypertension. More research is necessary to better understand this relationship.
Patients with connective-tissue diseases, namely the CREST (calcinosis cutis, Raynaud phenomenon, esophageal motility disorder, sclerodactyly, and telangiectasia) variant of scleroderma, systemic lupus erythematosus, and mixed connective-tissue disease, are also predisposed to developing IPAH-like disease. This is now termed associated PAH, or APAH.
The pathophysiologic nature of this predisposition is unclear. In the past, most experts used the term "secondary" pulmonary arterial hypertension for these diseases, indicating that, similar to IPAH, the process involves the precapillary circulation but is somehow caused by or at least associated with the underlying (predisposing) disease.
A study by Soon et al determined that unexplained iron deficiency is more prevalent in patients with idiopathic pulmonary artery hypertension than in those with chronic thromboembolic pulmonary hypertension (CTEPH).[8] Interleukin-6 (IL-6) may play a role in this difference in prevalence.
PreviousNextEtiologyThe strict definition of IPAH is pulmonary hypertension with no known cause. However, associations have been recognized (eg, connective-tissue diseases, liver cirrhosis, exposure to anorexigens and likely other alpha-adrenergic stimulants [eg, cocaine, amphetamines],[9] HIV infection). How these associated conditions predispose to or cause PAH remains unknown.
PreviousNextEpidemiologyIPAH is responsible for approximately 125-150 deaths per year in the United States and has an incidence rate of approximately 2-6 cases per million population per year. The incidence and prevalence of APAH are considerably higher than those of IPAH. The worldwide incidence of IPAH approximates that observed in the United States, but variations in prevalence exist worldwide. A registry of patients with IPAH in France found a prevalence of IPAH of about 6 cases per million population.[10] IPAH occurs at a female-to-male ratio ranging from 2-9:1, depending on the treatment center sampled. In the United States, the average female-to-male ratio reported in clinical trials and registries is close to 4:1. The reasons for this female predilection remain unknown.Typically, younger women of childbearing age develop IPAH. However, IPAH can also affect individuals in their fifth and sixth decades of life or older.[11]
PreviousNextPrognosisIPAH has no cure. Untreated IPAH leads to right-sided heart failure and death. Prior to the 1990s, therapeutic options were limited. The emergence of prostacyclin analogues, endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and other novel drug therapies has greatly improved the outlook for patients with IPAH and IPAH-like diseases.
For untreated IPAH, the estimated 3-year survival rate is approximately 41%. In one study of long-term continuous intravenous prostacyclin therapy, 3-year survival increased to approximately 63%.[12] With newer therapies, perhaps in combination, these figures are expected to improve further.
Data on long-term survival in patients treated with other pulmonary vascular therapies are emerging. Patients whose disease progresses and is unresponsive to medical treatments either undergo transplantation or die of progressive right-sided heart failure.
Using the largest registry of patients with PAH to date, the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL Registry), Benza et al analyzed factors determining survival in 2716 patients.[13] Using this data, they derived a multivariable, weighted risk formula incorporating 19 independent factors identified as having an impact on PAH patient survival, thus allowing clinicians to incorporate factors encountered in real-world management of PAH in their overall risk/severity assessment.
In another analysis of data from the REVEAL Registry, Frost et al found that PAH patients with mean pulmonary capillary wedge pressure (PCWP) of 16-18 mmHg at diagnostic right heart catheterization were heavier, older, and were more likely to have comorbidities associated with left ventricular diastolic dysfunction at diagnosis than patients with PCWP ≤15 mmHg. Five-year survival was poor in both PCWP subgroups.[14]
PreviousProceed to Clinical Presentation , Primary Pulmonary Hypertension





0 comments:
Post a Comment