Exercise testing is a cardiovascular stress test using treadmill bicycle exercise with ECG and blood pressure monitoring. Pharmacologic stress testing, established after exercise testing, is a diagnostic procedure in which cardiovascular stress induced by pharmacologic agents is demonstrated in patients with decreased functional capacity or in patients who cannot exercise. Pharmacologic stress testing is used in combination with imaging modalities such as radionuclide imaging and echocardiography.
Radionuclide uptake and ECG images are depicted below:
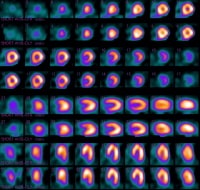 Normal radionuclide uptake (dipyridamole-Cardiolite).
Normal radionuclide uptake (dipyridamole-Cardiolite).  ECGs show a normal sinus rhythm and a sinus rhythm with a left bundle branch block.
ECGs show a normal sinus rhythm and a sinus rhythm with a left bundle branch block. 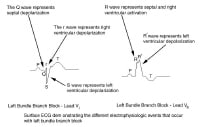 ECG depicts electrophysiologic events of left bundle branch block.
ECG depicts electrophysiologic events of left bundle branch block. Adenosine, dipyridamole (Persantine), and dobutamine are the most widely available pharmacologic agents for stress testing. Regadenoson, an adenosine analog, has a longer half-life than adenosine, and therefore a bolus versus continuous administration.
Adenosine, dipyridamole, and regadenosine are cardiac vasodilators. They dilate coronary vessels, which causes increased blood velocity and flow rate in normal vessels and less of a response in stenotic vessels. This difference in response leads to a steal of flow, and perfusion defects appear in cardiac nuclear scans or as ST-segment changes.
Dobutamine is a cardiac inotrope and chronotrope. The heart responds to dobutamine similarly to the way it responds to exercise.
AdenosineAdenosine is a naturally occurring substance found throughout the body in various tissues. It functions to regulate blood flow in many vascular beds, including the myocardium. The mechanisms by which adenosine is produced intracellularly are the S -adenosyl homocysteine and the adenosine triphosphate pathways; the latter plays a role during ischemia.
Once transported across cell membranes, adenosine interacts and activates the A1 and A2 cell surface receptors. In the vascular smooth muscles, adenosine primarily acts by activation of the A2 receptor, which stimulates adenylate cyclase, leading to an increase in cyclic adenosine monophosphate (cAMP) production. Increased cAMP levels inhibit calcium uptake by the sarcolemma, causing smooth muscle relaxation and vasodilation. Activation of the vascular A1 receptor also occurs, which stimulates guanylate cyclase, inducing cyclic guanosine monophosphate production, leading to vasodilation.
This direct coronary artery vasodilation induced by adenosine is attenuated in diseased coronary arteries, which have a reduced coronary flow reserve and cannot further dilate in response to adenosine. This is not the case in healthy or less-diseased coronary arteries in the same patient, which produces relative flow heterogeneity throughout the coronary arteries, resulting in relatively more coronary blood flow in the healthy or less-diseased coronary arteries compared with the more-diseased coronary artery. In most cases, coronary blood flow in the diseased coronary arteries does not decrease.
In cases of severe vessel stenosis or total occlusions with compensatory collateral circulation, a decrease in coronary blood flow may occur in the diseased coronary artery, thus inducing ischemia via a coronary steal phenomenon. This regional flow abnormality also induces a perfusion defect during radionuclide imaging.
Dipyridamole (Persantine)Dipyridamole is an indirect coronary vasodilator that works by increasing intravascular adenosine levels. This occurs by the inhibition of intracellular reuptake and deamination of adenosine. However, the increase in coronary blood flow induced by dipyridamole is less predictable than that of adenosine.
In one comparative study of dipyridamole and adenosine, 66% of patients (10 of 15) receiving dipyridamole versus 80% of patients (12 of 15) receiving adenosine had a maximal hyperemic response. However, this difference may not be apparent clinically. The mechanism of inducing a perfusion abnormality is similar to that of adenosine (see adenosine discussion above) except true coronary steal occurs more frequently.
DobutamineDobutamine is a synthetic catecholamine, which directly stimulates both beta-1 and beta-2 receptors. A dose-related increase in heart rate, blood pressure, and myocardial contractility occurs.
As with physical exertion, dobutamine increases regional myocardial blood flow based on physiological principles of coronary flow reserve. A similar dose-related increase in subepicardial and subendocardial blood flow occurs within vascular beds supplied by significantly stenosed arteries, with most of the increase occurring within the subepicardium rather than the subendocardium. Thus, perfusion abnormalities are induced by the development of regional myocardial ischemia.
Regadenoson (Lexiscan)Regadenoson is a new pharmacologic stress agent approved by the FDA in 2008 as an additional agent for use in stress testing for patients unable to perform the standard exercise stress test.[1, 2]
Regadenoson produces maximal hyperemia quickly and maintains it for an optimal duration that is practical for radionuclide myocardial perfusion imaging. Regadenoson's simple rapid bolus administration and short duration of hyperemic effect point to an advantage of enhanced control for the clinician.
Regadenoson is an agonist with low affinity (Ki ≈ 1.3 μM) for the A2A adenosine receptor, and at least a 10-fold lower affinity for the A1 adenosine receptor (Ki > 16.5 μM). In addition, it has relatively weak affinity for the A2B and A3 adenosine receptors.
Coronary vasodilation and an increase in coronary blood flow (CBF) results from activation of the A2A adenosine receptor by regadenoson.
NextIndicationsThe American College of Cardiology Foundation (ACCF) appropriateness utilization criteria (AUC) provide guidelines for appropriate testing. Pharmacologic stress testing is generally instituted when contraindications to routine exercise stress exist or when the patient is unable to exercise because of debilitating conditions in various forms. These include the following general indications:
Elderly patients with decreased functional capacity and possible CADPatients with chronic debilitation and possible CADYounger patients with functional impairment due to injury, arthritis, orthopedic problems, peripheral neuropathy, myopathies, or peripheral vascular disease, in which a maximal heart rate is not easily achieved with routine exercise stress testing, usually because of an early onset of fatigue due to musculoskeletal, neurologic, or vascular problems rather than cardiac ischemia Other cases, including patients taking beta-blockers or other negative chronotropic agents that would inhibit the ability to achieve an adequate heart response to exerciseIndications for specific pharmacologic agents are as follows:
AdenosineAny physical limitation that prevents a patient from exercising maximally is an indication for vasodilator stress testing.Patients taking beta-blockers or other negative chronotropic agents that would inhibit the ability to achieve an adequate heart rate response to exercise are also appropriate candidates for vasodilator stress. Patients with left bundle branch block or ventricular pacemaker (particularly those with severely diseased AV nodes or status post-AV node ablation who are unable to override their ventricular pacing rate) should undergo pharmacologic vasodilator stress because exercise stress often produces a false-positive perfusion defect in the interventricular septum. These defects are probably related to decreased septal contractility, which is accompanied by an autoregulated fall in coronary blood flow to the interventricular septum. Exercise stress or any other cause of tachycardia tends to enhance this heterogeneous perfusion by increasing the flow proportionately more in the normally contracting myocardium, resulting in a falsely underperfused interventricular septum on perfusion imaging. Vasodilator stress has been shown to overcome this coronary blood flow autoregulation, resulting in a more homogeneous perfusion pattern. Dipyridamole (Persantine)Any physical limitation that prevents a patient from exercising maximally is an indication for vasodilator stress.Patients taking beta-blockers or other negative chronotropic agents that would inhibit the ability to achieve an adequate heart rate response to exercise are also appropriate candidates for vasodilator stress. Patients with left bundle branch block or a ventricular pacemaker (particularly those with severely diseased AV nodes or status post-AV node ablation who are unable to override their ventricular pacing rate) should undergo vasodilator stress because exercise stress often produces a false-positive perfusion defect in the interventricular septum. These defects are probably related to decreased septal contractility, which is accompanied by an autoregulated decrease in coronary blood flow to the interventricular septum. Exercise stress or any other cause of tachycardia tends to enhance this heterogeneous perfusion by increasing the flow proportionately more in the normally contracting myocardium, resulting in a falsely underperfused interventricular septum with perfusion imaging. Vasodilator stress has been shown to overcome this coronary blood flow autoregulation, resulting in a more homogeneous perfusion pattern. DobutamineConsider dobutamine as a second-line pharmacologic stressor to be used in patients who cannot perform exercise stress and have a contraindication to vasodilator stress. Regadenoson (Lexiscan)Regadenoson injection is indicated for radionuclide myocardial perfusion imaging (MPI) in patients unable to undergo adequate exercise stress testing due to body habitus or other comorbidities as outlined in contraindications for exercise stress testing in Medscape Reference article Treadmill Stress Testing. PreviousNextContraindicationsCurrent AUC guidelines do not recommend routine testing within 2 years for patients who have undergone coronary revascularization procedures. However, one study has shown that 12% of these patients who visit their physician at least 3 months after the procedure undergo stress echocardiography testing within 30 days of the visit. The study shows discretionary stress testing is performed more frequently by physicians who bill for technical and professional fees compared to physicians who do not bill for these services, possibly as a way to recoup upfront costs for imaging equipment.[1]
Specific pharmacologic agents have specific contraindications, as follows:
AdenosineAbsolute
Patients with active bronchospasm or patients being treated for reactive airway disease should not be administered adenosine because this can lead to prolonged bronchospasm, which can be difficult to treat or can remain refractory. Patients with more than first-degree heart block (without a ventricular-demand pacemaker) should not undergo adenosine infusion because this may lead to worsening of the heart block. While this is usually transient, due to the extremely short half-life of adenosine (approximately 6 s), cases of prolonged heart block (and asystole) have been reported. Patients with an SBP less than 90 mm Hg should not undergo adenosine stress testing because of the potential for further lowering of the blood pressure. Patients using dipyridamole or methylxanthines (eg, caffeine and aminophylline) should not undergo an adenosine stress test because these substances act as competitive inhibitors of adenosine at the receptor level, potentially decreasing or completely attenuating the vasodilatory effect of adenosine. In general, patients should refrain from ingesting caffeine for at least 24 hours prior to adenosine administration. Patients should avoid decaffeinated products, which typically contain some caffeine, as opposed to caffeine-free products, which do not.Relative
Patients with a remote history of reactive airway disease (COPD/asthma) that has been quiescent for a long time (approximately 1 y) may be candidates for adenosine. However, if a question exists concerning the status of the patients' airway disease, a dobutamine stress test may be the safer choice. Patients with a history of sick sinus syndrome (without a ventricular-demand pacemaker) should undergo adenosine stress testing with caution. These patients are prone to significant bradycardia with adenosine; therefore, use caution if they are to undergo adenosine stress. Similarly, those patients with severe bradycardia (heart rate of 40 bpm) should undergo adenosine stress with caution. Dipyridamole (Persantine)Absolute
Patients with active bronchospasm or patients being treated for reactive airway disease should not be administered dipyridamole because this can lead to prolonged bronchospasm, which can be difficult to treat or can remain refractory. Patients with more than first-degree heart block (without a ventricular demand pacemaker) should not undergo dipyridamole infusion because this may lead to worsening of the heart block. Patients with an SBP of less than 90 mm Hg should not undergo dipyridamole stress testing because of the potential for further lowering of the blood pressure. Patients using methylxanthines (eg, caffeine, aminophylline) should not undergo dipyridamole stress testing because these substances act as competitive inhibitors of dipyridamole at the receptor level, potentially decreasing or completely attenuating the vasodilatory effect of dipyridamole. In general, patients should refrain from ingesting caffeine for at least 24 hours prior to dipyridamole administration. Patients should avoid decaffeinated products, which typically contain some caffeine, as opposed to caffeine-free products, which do not.Relative
Patients with a remote history of reactive airway disease (COPD/asthma) that has been quiescent for a long time (approximately 1 y) may be candidates for dipyridamole. However, if a question exists concerning the status of the patients' airway disease, dobutamine stress testing may be the safer choice. Patients with a history of sick sinus syndrome (without a ventricular demand pacemaker) should undergo dipyridamole stress testing with caution. These patients are prone to significant bradycardia with dipyridamole; therefore, use caution if they are to undergo dipyridamole stress. Similarly, those patients with severe bradycardia (heart rate 40 bpm) should undergo dipyridamole stress with caution. DobutaminePatients with recent (1 wk) myocardial infarction; unstable angina; significant aortic stenosis or obstructive cardiomyopathy; atrial tachyarrhythmias with uncontrolled ventricular response; history of ventricular tachycardia, uncontrolled hypertension, or thoracic aortic aneurysm; or left bundle branch block should not undergo dobutamine stress testing.
Regadenoson (Lexiscan)Regadenoson should not be administered to patients with second-degree atrioventricular block or sinus node dysfunction, unless these patients have a functioning artificial pacemaker.
PreviousNextTechnical ConsiderationsBest PracticesReview the patient's medication and caffeine intake:Theophylline can reduce ischemic changes on the ECG with vasodilator stress testing.Caffeine has been reported to reduce ischemic changes on ECG with vasodilator stress testing. However, one study demonstrated that one cup of coffee, one hour prior to stress testing did not attenuate the results of adenosine nuclear imaging.[3] Calcium channel blockers, beta-blockers, and nitrates can also alter perfusion defects on pharmacologic stress tests and therefore ideally should be withheld for 24 hours prior to pharmacologic stress testing. Dipyridamole and adenosine can lead to bronchospasm; they are generally avoided in patients with severe reactive airway disease or active wheezing. Dobutamine is safe to use in these patients.Instruct patients with diabetes regarding insulin requirements.
Complication PreventionThe American College of Cardiology/American Heart Association Clinical Competence Statement on Stress Testing emphasizes the importance of knowledge of possible complications and rates of complications for particular agents for patients and those supervising stress tests. The following guidelines are of particular importance:
Avoid contraindications.Do not exceed standard dosages.Perform tests only after informed consent has been obtained.Ensure an attending physician is present.Retain outpatients for 60 minutes after testing.Ensure indications for testing are met.PreviousNextOutcomesStress testing does not successfully identify all high-risk patients.
The table below depicts findings and results for stress testing.
Table 1. Findings and Likely Associated Results (Open Table in a new window)
ResultsRestStressConclusionFindingsNormalNormal Blood flow to coronary artery is likely normalFindingsNormalReversible perfusion defectArtery blockage may be presentFindingsAbnormalAbnormalHeart has had prior injury, eg, previous heart attackPotential findings are illustrated in the images below:
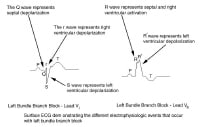 ECG depicts electrophysiologic events of left bundle branch block. PreviousProceed to Periprocedural Care , Pharmacologic Stress Testing
ECG depicts electrophysiologic events of left bundle branch block. PreviousProceed to Periprocedural Care , Pharmacologic Stress Testing






0 comments:
Post a Comment