Sudden cardiac death (SCD) is an unexpected death due to cardiac causes that occurs in a short time period (generally within 1 hour of symptom onset) in a person with known or unknown cardiac disease. It is estimated that more than 7 million lives per year are lost to SCD worldwide, including over 300,000 in the United States.
Essential update: Fibrosis predicts sudden cardiac death in dilated cardiomyopathyMidwall fibrosis is an independent predictor of mortality and SCD in patients with nonischemic dilated cardiomyopathy, according to a prospective, longitudinal study by Gulati et al. Of 472 patients with dilated cardiomyopathy, 38 of 142 patients with fibrosis (26.8%) died, compared to 35 of 330 patients without fibrosis (10.6%), over a median follow-up period of 5.3 years. Adjusting for conventional prognostic factors, including left ventricular ejection fraction (LVEF), the investigators found that the presence and extent of fibrosis were independently associated with the risk of cardiovascular mortality and cardiac transplantation.[1, 2]
Signs and symptomsPatients at risk for SCD may have prodromes of chest pain, fatigue, palpitations, and other nonspecific complaints. Factors relating to the development of coronary artery disease (CAD) and, subsequently, myocardial infarction (MI) and ischemic cardiomyopathy include the following:
Family history of premature coronary artery diseaseSmokingDyslipidemiaHypertensionDiabetesObesitySedentary lifestyleSpecific factors relating to cardiovascular disease are listed below.
Coronary artery disease
Previous cardiac arrestSyncopePrior myocardial infarction, especially within 6 monthsEjection fraction of less than 30-35%History of frequent ventricular ectopy: More than 10 premature ventricular contractions (PVCs) per hour or nonsustained ventricular tachycardia (VT)Dilated cardiomyopathy
Previous cardiac arrestSyncopeEjection fraction of less than 30-35%Use of inotropic medicationsHypertrophic cardiomyopathy
Previous cardiac arrestSyncopeFamily history of SCDSymptoms of heart failureDrop in systolic blood pressure (SBP) or ventricular ectopy upon stress testingPalpitationsMost persons are asymptomaticValvular disease
Valve replacement within past 6 monthsSyncopeHistory of frequent ventricular ectopySymptoms associated with severe, uncorrected aortic stenosis or mitral stenosisLong QT syndrome
Family history of long QT and SCDMedications that prolong the QT intervalBilateral deafnessSee Clinical Presentation for more detail.
DiagnosisLaboratory studies
Cardiac enzymes (creatine kinase, myoglobin, troponin)Electrolytes, calcium, and magnesiumQuantitative drug levels (quinidine, procainamide, tricyclic antidepressants, digoxin): High or low drug levels may have a proarrhythmic effect Toxicology screen: For drugs, such as cocaine, that cause vasospasm-induced ischemiaThyroid-stimulating hormoneBrain natriuretic peptide (BNP)Other tests to evaluate or predict risk of SCD
Imaging studies: Chest radiography, echocardiography, nuclear scintigraphyElectrocardiography (ECG): Including, possibly, signal-averaged ECGCoronary angiographyElectrophysiologySee Workup for more detail.
ManagementIn general, advanced cardiac life support (ACLS) guidelines should be followed in all cases of sudden cardiac arrest (SCA).
Bystander cardiopulmonary resuscitation (CPR)
Immediate chest compression and defibrillation are reportedly the most important interventions to improve the outcome in SCA. Research indicates that bystander use of automated external defibrillators increases neurologically intact survival to discharge (14.3% without bystander defibrillation; 49.6% with defibrillation).[3]
Pharmacologic therapy
Medications used in SCD include the following:
Ventricular arrhythmia: Epinephrine or vasopressin; amiodarone and lidocaine can be used as antiarrhythmic drugs if defibrillation does not control the arrhythmia Pulseless electrical activity (PEA): Epinephrine; atropine used in case of bradycardiaAsystole: One study suggested that vasopressin is more effective in acute therapy for asystole than epinephrine[4] Medical stabilization: Empiric beta blockers are reasonable in many circumstancesTherapeutic hypothermia
This intervention limits neurologic injury associated with brain ischemia during a cardiac arrest and reperfusion injury associated with resuscitation.[5]
Surgery
Temporary cardiac pacingRadiofrequency ablationCardioverter defibrillator therapyCoronary artery bypass grafting (CABG)Excision of ventricular tachycardia fociExcision of left ventricular aneurysmsAortic valve replacementOrthotopic heart transplantationSee Treatment for more detail.
Image library Interplay of various risk factors that can lead to sudden cardiac death. NextBackground
Interplay of various risk factors that can lead to sudden cardiac death. NextBackgroundSudden cardiac death (SCD) is an unexpected death due to cardiac causes occurring in a short time period (generally within 1 h of symptom onset) in a person with known or unknown cardiac disease. Most cases of SCD are related to cardiac arrhythmias. Approximately half of all cardiac deaths can be classified as SCDs. SCD represents the first expression of cardiac disease in many individuals who experience out-of-hospital cardiac arrest.
This article explores the epidemiology and pathophysiology of SCD. It also discusses the diagnostic approach to patients at risk for SCD, as well as the prevention of SCD and the treatment of sudden cardiac arrest.
PreviousNextPathophysiologyThe most common electrophysiologic mechanisms leading to SCD are tachyarrhythmias such as ventricular fibrillation (VF) or ventricular tachycardia (VT). Interruption of tachyarrhythmias, using either an automatic external defibrillator (AED) or an implantable cardioverter defibrillator (ICD), has been shown to be an effective treatment for VF and VT.[6] The implantable defibrillator has become the central therapeutic factor in the prevention and treatment of sudden cardiac death. Patients with tachyarrhythmias, especially VT, carry the best overall prognosis among patients with sudden cardiac arrest (SCA).
There are multiple factors at the organ (eg imbalance of autonomic tone), tissue (eg reentry, wave break, and action potential duration alternans), cellular (eg triggered activity, and automaticity) and subcellular (abnormal activation or deactivation of ion channels) level involved in generation of VT or VF in different conditions. An anatomical or a functional block in the course of impulse propagation may create a circuit with the wave front circling around it and resulting in VT. Other mechanisms such as wave break and collisions are involved in generating VF from VT. While at the tissue level the above-mentioned reentry and wave break mechanisms are the most important known mechanisms of VT and VF, at the cellular level increased excitation or decreased repolarization reserve of cardiomyocytes may result in ectopic activity (eg automaticity, triggered activity), contributing to VT and VF initiation.
At the subcellular level, altered intracellular Ca2+ currents, altered intracellular K+ currents (especially in ischemia), or mutations resulting in dysfunction of a sodium channel (Na+ channelopathy) can increase the likelihood of VT and VF.
Approximately 20-30% of patients with documented sudden death events have bradyarrhythmia or asystole at the time of initial contact. Oftentimes, it is difficult to determine with certainty the initiating event in a patient presenting with a bradyarrhythmia because asystole and pulseless electrical activity (PEA) may result from a sustained VT. Less commonly, an initial bradyarrhythmia producing myocardial ischemia may then provoke VT or VF.
Most cases of SCD occur in patients with structural abnormalities of the heart. Myocardial infarction (MI) and post-MI remodeling of the heart is the most common structural abnormality in patients with SCD. In patients who survive a myocardial infarction, the presence of premature ventricular contractions (PVCs), particularly complex forms such as multiform PVCs, short coupling intervals (R-on-T phenomenon), or VT (salvos of 3 or more ectopic beats), reflect an increased risk of sudden death. However suppression of the PVCs with antiarrhythmic drugs increases mortality, owing to the proarrhythmic risk of currently available medications.
Hypertrophic cardiomyopathy and dilated cardiomyopathy are associated with an increased risk of SCD. Various valvular diseases such as aortic stenosis are associated with increased risk of SCD. Acute illnesses, such as myocarditis, may provide both an initial and sustained risk of SCD due to inflammation and fibrosis of the myocardium.
Less commonly, SCD happens in patients who may not have apparent structural heart disease. These conditions are usually inherited arrhythmia syndromes.
Even though many patients have anatomic and functional cardiac substrates that predispose them to develop ventricular arrhythmias, only a small percentage develop SCD. Identifying the patients at risk for SCD remains a challenge. The strongest known predictor of SCD is significant left ventricular dysfunction of any cause. The interplay between the regional ischemia, LV dysfunction, and transient inciting events (eg, worsened ischemia, acidosis, hypoxemia, wall tension, drugs, metabolic disturbances) has been proposed as being the precipitator of sudden death (see the image below).
 Interplay of various risk factors that can lead to sudden cardiac death. PreviousNextEpidemiologyFrequencyUnited States
Interplay of various risk factors that can lead to sudden cardiac death. PreviousNextEpidemiologyFrequencyUnited StatesSCD accounts for approximately 325,000 deaths per year in the United States; more deaths are attributable to SCD than to lung cancer, breast cancer, or AIDS. This represents an incidence of 0.1-0.2% per year in the adult population. SCD is often the first expression of CAD and is responsible for approximately 50% of deaths from CAD.
In several population-based studies, the incidence of out-of-hospital cardiac arrest has been noted as declining in the past 2 decades, but the proportion of sudden CAD deaths in the United States has not changed. A high incidence of SCD occurs among certain subgroups of high-risk patients (congestive heart failure with ejection fraction
InternationalThe frequency of SCD in Western industrialized nations is similar to that in the United States. The incidence of SCD in other countries varies as a reflection of the prevalence of coronary artery disease or other high-frequency cardiomyopathies in those populations. The trend toward increasing SCD events in developing nations of the world is thought to reflect a change in dietary and lifestyle habits in these nations. It has been estimated that SCD claims more than 7,000,000 lives per year worldwide.[7]
Mortality/MorbidityOf more than 300,000 deaths attributed to SCD in the United States each year, a large portion (as many as 40%) are unwitnessed. For most people who experience SCD, their survival depends on the presence of individuals who are competent in performing basic life support, the rapid arrival of personnel and apparatus for defibrillation and advanced life support, and transfer to a hospital. Even under ideal circumstances, only an estimated 20% of patients who have out-of-hospital cardiac arrest survive to hospital discharge. In a study of out-of-hospital cardiac arrest survival in New York City, only 1.4% of patients survived to hospital discharge. Other studies in suburban and rural areas have indicated higher rates of survival (as high as 35%). Placement of automatic external defibrillators throughout communities and training people to use them has the potential to markedly improve outcomes from SCD.
Upon emergency department (ED) presentation, the most important determinants of survival include (1) an unsupported systolic blood pressure (SBP) greater than 90 mm Hg, (2) a time from loss of consciousness to return of spontaneous circulation (ROSC) of less than 25 minutes, and (3) some degree of neurological responsiveness. A major adverse outcome from a SCD event is anoxic encephalopathy, which occurs in 30-80% of cases.RaceMost studies demonstrate inconclusive data with regard to racial differences as they relate to the incidence of sudden death. Some studies suggest that a greater proportion of coronary deaths were "sudden" in blacks compared to whites. In a report by Gillum et al on SCD from 1980-1985, the percentage of coronary artery disease deaths occurring out of the hospital and in EDs was found to be higher in blacks than in whites (see the image below).[8]
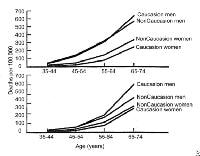 Cardiac death, sudden. Plots of mortality rates (deaths per 1000 persons) for ischemic heart disease occurring out of the hospital or in the emergency department (top) and occurring in the hospital (bottom) by age, sex, and race in 40 states during 1985. Sex
Cardiac death, sudden. Plots of mortality rates (deaths per 1000 persons) for ischemic heart disease occurring out of the hospital or in the emergency department (top) and occurring in the hospital (bottom) by age, sex, and race in 40 states during 1985. SexMen have a higher incidence of SCD than women, with a ratio of 3:1. This ratio generally reflects the higher incidence of obstructive coronary artery disease in men. Recent evidence suggests that a major sex difference may exist in the mechanism of myocardial infarction. Basic and observational data point to the fact that men tend to have coronary plaque rupture, while women tend to have plaque erosion. Whether this biologic difference accounts for the male predominance of SCD is unclear.
AgeThe incidence of SCD parallels the incidence of coronary artery disease, with the peak of SCD occurring in people aged 45-75 years. The incidence of SCD increases with age in men, women, whites, and nonwhites as the prevalence of coronary artery disease increases with age. However, the proportion of deaths that are sudden from coronary artery disease decreases with age. In the Framingham study, the proportion of coronary artery disease deaths that were sudden was 62% in men aged 45-54 years, but this percentage fell to 58% in men aged 55-64 years and to 42% in men aged 65-74 years.[9] According to Kuller et al, 31% of deaths are sudden in people aged 20-29 years.[10]
PreviousProceed to Clinical Presentation , Sudden Cardiac Death





0 comments:
Post a Comment