In 1930, Wolff, Parkinson, and White described a series of young patients who experienced paroxysms of tachycardia and had characteristic abnormalities on electrocardiography (ECG).[1] Currently, Wolff-Parkinson-White (WPW) syndrome is defined as a congenital condition involving abnormal conductive tissue between the atria and the ventricles that provides a pathway for a reentrant tachycardia circuit.
Essential update: New treatment study of children with WPWIrrigated-tip catheters have been used for ablation of accessory pathways in adults with WPW syndrome, but the safety of this technique in children has been in question. In a prospective study of consecutive patients younger than 18 years, Gulletta et al achieved overall procedural success after the first procedure in 39 of 41 cases (95%), with no complications and no recurrences. Mean procedure time was 26.4 minutes, and mean fluoroscopy time was 12.2 minutes.[24]
Signs and symptomsClinical manifestations of WPW syndrome may have their onset at any time from childhood to middle age, and they can vary in severity from mild chest discomfort or palpitations with or without syncope to severe cardiopulmonary compromise and cardiac arrest. Presentation varies by patient age.
Infants may present with the following:
TachypneaIrritabilityPallorIntolerance of feedingsEvidence of congestive heart failure if the episode has been untreated for several hoursA history of not behaving as usual for 1-2 daysAn intercurrent febrile illness may be presentA verbal child with WPW syndrome usually reports the following:
Chest painPalpitationsBreathing difficultyOlder patients can usually describe the following:
Sudden onset of a pounding heartbeatPulse that is regular and “too rapid to countâ€Typically, a concomitant reduction in their tolerance for activityPhysical findings include the following:
Normal cardiac examination findings in the vast majority of casesDuring tachycardic episodes, the patient may be cool, diaphoretic, and hypotensiveCrackles in the lungs from pulmonary vascular congestionIn many young patients, only minimal symptoms (eg, palpitations, weakness, mild dizziness) despite exceedingly fast heart ratesClinical features of associated cardiac defects may be present, such as the following:
CardiomyopathyEbstein anomalyHypertrophic cardiomyopathy (AMPK mutation)[8]See Clinical Presentation for more detail.
DiagnosisRoutine blood studies may be needed to help rule out noncardiac conditions triggering tachycardia. These may include the following:
Complete blood countChemistry panel, with renal function studies and electrolytesLiver function testsThyroid panelDrug screeningThe diagnosis of WPW syndrome is typically made with formal ECG monitoring (eg, telemetry, Holter monitoring) in conjunction with clues from the history and physical examination. Although the ECG morphology varies widely, the classic ECG features are as follows:
A shortened PR intervalA slurring and slow rise of the initial upstroke of the QRS complex (delta wave)A widened QRS complex (total duration >0.12 seconds)ST segment–T wave changes, generally directed opposite the major delta wave and QRS complexEchocardiography is needed for the following:
Evaluation of left ventricular (LV) function and wall motion abnormalitiesExcluding cardiomyopathy and an associated congenital heart defect (eg, hypertrophic cardiomyopathy, Ebstein anomaly, L-transposition of the great vessels)Stress testing is ancillary and may be used for the following:
To reproduce a transient paroxysmal dysrhythmiaTo document the relationship of exercise to the onset of tachycardiaTo evaluate the efficacy of antiarrhythmic drug therapyElectrophysiologic studies (EPS) can be used in patients with WPW syndrome to determine the following:
The mechanism of the clinical dysrhythmiaThe electrophysiologic properties (eg, conduction capability, refractory periods) of the accessory pathway and the normal atrioventricular (AV) nodal and His Purkinje conduction system The number and locations of accessory pathways (necessary for catheter ablation)The response to pharmacologic or ablation therapySee Workup for more detail.
ManagementTreatment of WPW dysrhythmias comprises the following:
Radiofrequency ablation of the accessory pathwayAntiarrhythmic drugs to slow accessory pathway conductionAV nodal blocking medications to slow AV nodal conductionAddressing the triggers that perpetuate the dysrhythmia, which include coronary heart disease, ischemia, cardiomyopathy, pericarditis, electrolyte disturbances, thyroid disease, and anemiaTermination of acute episodes
Narrow-complex AV reentrant tachycardia (AVRT) and AV nodal reentrant tachycardia (AVNRT) are treated by blocking AV node conduction with the following:
Vagal maneuvers (eg, Valsalva maneuver, carotid sinus massage, splashing cold water or ice water on the face)IV adenosine 6-12 mg via a large-bore line (the drug has a very short half-life)IV verapamil 5-10 mg or diltiazem 10 mgAtrial flutter/fibrillation or wide-complex tachycardia is treated as follows:
IV procainamide or amiodarone if wide-complex tachycardia is present, ventricular tachycardia (VT) cannot be excluded, and the patient is stable hemodynamically IbutilideThe initial treatment of choice for hemodynamically unstable tachycardia is direct current synchronized electrical cardioversion, biphasic, as follows:
A level of 100 J (monophasic or lower biphasic) initiallyIf necessary, a second shock with higher energy (200 J or 360 J)Radiofrequency ablation
Radiofrequency ablation is indicated in the following patients:
Patients with symptomatic AVRTPatients with AF or other atrial tachyarrhythmias that have rapid ventricular response via an accessory pathway (preexcited AF) Patients with AVRT or AF with rapid ventricular rates found incidentally during EPS for unrelated dysrhythmia, if the shortest preexcited RR interval during AF is less than 250 ms Asymptomatic patients with ventricular preexcitation whose livelihood, profession, insurability, or mental well-being may be influenced by unpredictable tachyarrhythmias or in whom such tachyarrhythmias would endanger the public safety[20] Patients with WPW and a family history of sudden cardiac deathSurgical treatment
Radiofrequency catheter ablation has virtually eliminated surgical open heart treatments in the vast majority of WPW patients, with the following exceptions:
Patients in whom RF catheter ablation (with repeated attempts) failsPatients undergoing concomitant cardiac surgery (possible exception)Patients with other tachycardias with multiple foci who require surgical intervention (very rare)Long-term antiarrhythmic therapy
Oral medication is the mainstay of therapy in patients not undergoing radiofrequency ablation, although the response to long-term antiarrhythmic therapy for the prevention of further episodes of tachycardia in patients with WPW syndrome remains quite variable and unpredictable. Choices include the following:
Dual-drug therapy (eg, procainamide and verapamil [class Ia and IV])Class Ic drugs (eg, flecainide, propafenone), typically used with an AV nodal blocking agentClass III drugs (eg, amiodarone, sotalol)In pregnancy, sotalol (class B) or flecainide (class C)See Treatment and Medication for more detail.
Image library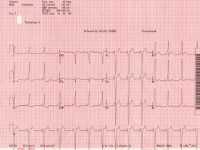 Classic Wolff-Parkinson-White electrocardiogram with short PR, QRS >120 ms, and delta wave. NextBackground
Classic Wolff-Parkinson-White electrocardiogram with short PR, QRS >120 ms, and delta wave. NextBackgroundIn 1930, Wolff, Parkinson, and White described a series of young patients who had a bundle branch block pattern on electrocardiography (ECG) findings, a short PR interval, and paroxysms of tachycardia.[1] Case reports began appearing in the literature in the late 1930s and early 1940s, and the term Wolff-Parkinson-White (WPW) syndrome was coined in 1940.
Preexcitation was defined by Durrer et al in 1970 with the following statement, "Preexcitation exists, if in relation to atrial events, the whole or some part of the ventricular muscle is activated earlier by the impulse originating from the atrium than would be expected if the impulse reached the ventricles by way of the normal specific conduction system only."[2]
WPW syndrome is currently defined as a congenital abnormality involving the presence of abnormal conductive tissue between the atria and the ventricles in association with supraventricular tachycardia (SVT). It involves preexcitation, which occurs because of conduction of an atrial impulse not by means of the normal conduction system, but via an extra atrioventricular (AV) muscular connection, termed an accessory pathway (AP), that bypasses the AV node.[3, 4]
Classic ECG findings that are associated with WPW syndrome include the following:
Presence of a short PR interval (A wide QRS complex longer than 120 ms with a slurred onset of the QRS waveform producing a delta wave in the early part of QRS Secondary ST-T wave changes (see the image below)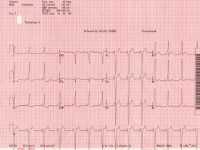 Classic Wolff-Parkinson-White electrocardiogram with short PR, QRS >120 ms, and delta wave.
Classic Wolff-Parkinson-White electrocardiogram with short PR, QRS >120 ms, and delta wave. Patients with WPW syndrome are potentially at an increased risk of dangerous ventricular arrhythmias due to extremely fast conduction across the bypass tract if they develop atrial flutter or atrial fibrillation (AF).
Some patients have a concealed bypass tract. Although they have an accessory AV connection, it lacks antegrade conduction; accordingly, these patients do not have the classic abnormalities of the surface ECG.
Only a small percentage of patients with WPW syndrome (sudden cardiac death (SCD). In patients who present with preexcited AF, cardiac electrophysiologic studies and radiofrequency (RF) catheter ablation may be curative. Other presentations include symptomatic SVT, which can also be cured by catheter ablation. Asymptomatic patients need periodic observation. The onset of cardiac arrhythmias, and possibly the sudden death risk, may be eliminated by prophylactic catheter ablation as well.[5]
This review discusses the pathogenesis, clinical presentation, evaluation, and treatment of patients with WPW syndrome.
Go to Management of Acute Wolff-Parkinson-White Syndrome for complete information on this topic.
PreviousNextPathophysiologyAccessory pathways or connections between the atrium and ventricle are the result of anomalous embryonic development of myocardial tissue bridging the fibrous tissues that separate the two chambers. This allows electrical conduction between the atria and ventricles at sites other than the AV node. Passage through APs circumvents the usual conduction delay between the atria and ventricles, which normally occurs at the AV node, and predisposes the patient to develop tachydysrhythmias.
Although dozens of locations for bypass tracts can exist in preexcitation, including atriofascicular, fasciculoventricular, nodofascicular, or nodoventricular, the most common bypass tract is an accessory atrioventricular (AV) pathway otherwise known as a Kent bundle. This is the anomaly seen in WPW syndrome. The primary feature that differentiates WPW syndrome from other AP-mediated supraventricular tachycardias (SVTs) is the ability of the AP to conduct in either an antegrade (ie, from atrium to ventricles) or a retrograde manner.
The presence of an AP allows a reentrant tachycardia circuit to be established. This reentrant mechanism is the typical cause of the SVT of which patients with preexcitation are at risk. The genesis of reentrant SVT involves the presence of dual conducting pathways between the atria and the ventricles[6] :
The natural AV nodal His-Purkinje tractOne or more AV accessory tract(s) (ie, AV connection or AP, Kent fibers, Mahaim fibers)These pathways usually exhibit different conduction properties and refractory periods that facilitate reentry. The effective refractory period (ERP, the time necessary for the electrical recovery needed to conduct the next impulse) of the accessory tract is often longer than that of the normal AV nodal His-Purkinje tract and requires time for conduction to recover before allowing reentry.
The degree of preexcitation on a surface ECG in a person with WPW pattern can be estimated by the width of the QRS and the length of the PR interval. A wider or more preexcited QRS with a short PR interval with absent or nearly absent isoelectric component reveals that most (or all) of the ventricular depolarization initiates through the AP insertion rather than through the AV node/His Purkinje system.
However, the QRS width may vary, becoming narrower during more rapid heart rates. This is possible because catecholamines permit the AV node to contribute more (or entirely) to ventricular depolarization by enhancing AV node conduction.
Types of SVT include orthodromic tachycardia (down the AV nodal His-Purkinje system and retrograde conduction up an AP), orthodromic tachycardia with a concealed AP (retrograde conduction only), and antidromic tachycardia (down the AP and retrograde conduction up the His-Purkinje system and AV node). In patients with WPW in which the AP participates, 95% of SVT is due to orthodromic tachycardia and 5% is due to antidromic tachycardia.
Orthodromic tachycardiaWhen a premature ectopic atrial impulse advances towards the ventricle, it may block at the AP but conduct in down the normal AVN/His Purkinje pathway. The impulse then reenters the AP in a retrograde fashion to perpetuate a circus movement of the impulse. Such reentrant tachycardia is described as orthodromic. Premature ventricular contractions (PVCs) can also initiate orthodromic tachycardia.
In orthodromic tachycardia, the normal pathway is used for ventricular depolarization, and the AP is used for the retrograde conduction essential for reentry. On ECG findings, the delta wave is absent, the QRS complex is normal, and P waves are typically inverted in the inferior and lateral leads.
Orthodromic tachycardia with concealed accessory pathwaySome APs are unable to conduct in an antegrade fashion. These are called concealed APs (as in concealed WPW syndrome) because manifest preexcitation is considered to be a pattern visible on the usual surface ECG. They account for about 30% of all SVTs induced on EPS.
Although no evidence of the pathway is present during sinus rhythm (ie, no preexcitation), orthodromic tachycardias can occur. Orthodromic tachycardia may also occur when there are 2 or more accessory connections, and in that case, the retrograde conduction may occur through the AV node, through one of the accessory connections, or through both.
This type of SVT may be difficult to distinguish from the usual AV nodal reentrant tachycardia (AVNRT) on the standard surface ECG. If the heart rate is higher than 200 bpm with QRS alternans and a retrograde P wave visible in the ST segment (long R-P tachycardia) following the QRS complex, a concealed AP may be the diagnosis. This determination is most accurately made with EPS.
Antidromic tachycardiaLess commonly, a shorter refractory period in the AP may cause blockade of an ectopic atrial impulse in the normal pathway, with antegrade conduction down the AP and then retrograde reentry of the normal AV nodal pathway. This type of tachycardia is called antidromic tachycardia.
On ECG, the QRS is wide, reflecting an exaggeration of the delta wave during sinus rhythm (ie, wide-QRS tachycardia). Such tachycardias are difficult to differentiate from ventricular tachycardias and often have a slurred R wave upstroke with QRS duration longer than 160 ms.
Only about 5% of the tachycardias in patients who have WPW syndrome are antidromic tachycardias; the remaining 95% are orthodromic. Even when the AP conducts solely in a retrograde fashion, it can still participate in the reentrant circuit and produce an orthodromic AV reciprocating tachycardia with a narrow QRS morphology. The presence of an antidromic tachycardia should prompt a careful search for a second bypass tract.
Lown-Ganong-Levine syndromeAnother common preexcitation syndrome, Lown-Ganong-Levine (LGL) syndrome, also has an AP—the James fibers, which connect the atria serially to the His bundle. This leads to accelerated conduction to the ventricle without QRS widening, as the distal pathway remains the His Purkinje system. This pathway is not typically involved in re-entrant tachycardias, and is observed clinically.
PreviousNextEtiologyAPs are considered congenital phenomena that are related to a failure of insulating tissue maturation within the AV ring—even though their manifestations are often detected in later years, making them appear to be acquired.
Family studies, as well as recent molecular genetic investigations, indicate that WPW syndrome, along with associated preexcitation disorders, may have a genetic component. It may be inherited as a familial trait, with or without associated congenital heart defects (CHDs)[7] ; 3.4% of those with WPW syndrome have first-degree relatives with preexcitation.
The familial form is usually inherited as a Mendelian autosomal dominant trait. Although rare, mitochondrial inheritance has also been described. The syndrome may also be inherited with other cardiac and noncardiac disorders, such as familial atrial septal defects, familial hypokalemic periodic paralysis, and tuberous sclerosis.
Clinicians have long recognized the association of WPW syndrome with autosomal dominant familial hypertrophic cardiomyopathy. However, only comparatively recently was a genetic substrate linking hypertrophic cardiomyopathy to WPW syndrome and skeletal myopathy described.[8]
Patients with mutations in the gamma 2 subunit of adenosine monophosphate (AMP)-activated protein kinase (PRKAG2) develop cardiomyopathy characterized by ventricular hypertrophy, WPW syndrome, AV block, and progressive degenerative conduction system disease. The mutation is believed to produce disruption of the annulus fibrosus by accumulation of glycogen within myocytes, which causes preexcitation. This is thought to be the case in Pompe disease, Danon disease, and other glycogen-storage diseases.
Infantile Pompe disease or glycogen-storage disease type II is a fatal genetic muscle disorder that is caused by deficiency of acid alpha-glucosidase (GAA). These patients have a shortened PR interval, large left ventricular (LV) voltages, and an increased QT dispersion (QTd).
Mutations in the lysosome-associated membrane protein 2 (LAMP2), which cause accumulation of cardiac glycogen, are thought to be the etiology of a significant number of hypertrophic cardiomyopathies in children, especially when skeletal myopathy, WPW syndrome, or both are present.
For example, Danon disease is an X-linked lysosomal cardioskeletal myopathy; males are more often and more severely affected than females. It is caused by mutations in the LAMP2 that produce proximal muscle weakness and mild atrophy, left ventricle hypertrophy, WPW syndrome, and mental retardation.
Patients with the Ebstein anomaly may develop WPW syndrome. They frequently have multiple accessory bypass tracts, mostly on the right, in the posterior part of the septum or the posterolateral wall of the right ventricle. The orthodromic reciprocating tachycardia in such patients often exhibits right bundle-branch block (RBBB) and a long ventriculoatrial (VA) interval.
Preexcitation can be surgically created, as in certain types of Bjork modifications of the Fontan procedure, if atrial tissue is flapped onto and sutured to ventricular tissue. Certain tumors of the AV ring, such as rhabdomyomas, may also cause preexcitation.
PreviousNextEpidemiologyUnited States statisticsThe prevalence of ventricular preexcitation is thought to be 0.1-0.3%, or 1 to 3 per 1000 people in the general population. Estimates of arrhythmia incidence in patients with preexcitation vary widely, ranging from 12% to 80% in several surveys.
The incidence of preexcitation and WPW syndrome ranges from 0.1 to 3 cases per 1000 population (average, 1.5 cases per 1000 population) in otherwise healthy persons. This includes only patients with manifest preexcitation (delta wave evident on surface 12-lead ECG). About 60-70% of these individuals have no other evidence of heart disease. Approximately 4 newly diagnosed cases of WPW syndrome per 100,000 population occur each year.
In a review of ECG findings from 22,500 healthy aviation personnel, 0.25% exhibited findings consistent with the WPW pattern, with a 1.8% reported incidence of tachycardia.
The location of the APs, in descending order of frequency, is (1) 53%, the left free wall, (2) 36%, posteroseptal, (3) 8%, right free wall, and (4) 3%, anteroseptal. The presence of concealed APs accounts for approximately 30% of patients with apparent SVT referred for EPS. These patients do not have true WPW syndrome because no delta wave is present, but they do have the potential for orthodromic tachycardia.
Approximately 80% of patients with WPW syndrome have a reciprocating tachycardia, 15-30% will develop AF, and 5% have atrial flutter. Ventricular tachycardia is uncommon. Patients with mitral valve prolapse have an association with WPW, but the mechanism is unclear.
International statisticsWorldwide, the incidence and prevalence of WPW syndrome parallel those seen in the United States.
Age-related differences in incidenceWPW syndrome is found in persons of all ages. Most patients with WPW syndrome present during infancy. However, a second peak of presentation is noted in school-aged children and in adolescents. This interesting bimodal age distribution is due to permanent or transitory loss of preexcitation during infancy in some patients and during late adolescence in others.
The prevalence of WPW syndrome decreases with age as a consequence of apparent attenuation of conduction speed in the AP. About one fourth of patients lose preexcitation over a 10-year period, probably as a result of fibrotic changes at the site of insertion of the accessory bypass tract with loss of electrical conduction properties between cardiac chambers. Cases have been described in which ECG evidence of preexcitation disappears completely. One tenth of patients with concealed APs lose retrograde conduction over 10 years.
In asymptomatic patients, antegrade conduction across the accessory pathway (AP) may spontaneously disappear with advancing age (one fourth of patients lose antegrade bypass tract conduction over 10 years).
In patients with abnormal ECG findings indicative of WPW syndrome, the frequency of SVT paroxysms increases from 10% in people aged 20-39 years to 36% in people older than 60 years.[9] Overall, about 50% of patients with WPW develop tachyarrhythmias.
Sex-related differences in incidenceWPW pattern appears to affect the 2 sexes equally; however, WPW syndrome has been found to be more frequent in males. One study documented a male-to-female ratio of approximately 2:1. Another reported 1.4 cases of WPW syndrome per 1000 men and 0.9 cases per 1000. A third study found a 3.5-fold higher prevalence of WPW syndrome in men.
Race-related differences in incidenceNo clear racial predilection appears to exist.
PreviousNextPrognosisOnce identified and appropriately treated, WPW syndrome is associated with an excellent prognosis, including the potential for permanent cure through RF catheter ablation.
Asymptomatic patients with only preexcitation on ECG generally have a very good prognosis. Many develop symptomatic arrhythmias over time, which can be prevented with prophylactic EPS and RF catheter ablation. Patients with a family history of SCD or significant symptoms of tachyarrhythmias or cardiac arrest have worse prognoses. However, once definitive therapy is performed, including curative ablation, the prognosis is once again excellent.
Noninvasive risk stratification can be useful if abrupt loss of preexcitation occurs with exercise or procainamide infusion.
Mortality in WPW syndrome is rare and is related to SCD. The incidence of SCD in WPW syndrome is approximately 1 in 100 symptomatic cases when followed for up to 15 years. Although relatively uncommon, SCD may be the initial presentation in as many as 4.5% of cases.
Even in patients with asymptomatic WPW, the risk of SCD is increased above that of the general population. Medical therapy with agents such as digoxin may increase this risk if the patient has AF or atrial flutter. The risk in asymptomatic patients is low and can be reduced further with prophylactic catheter ablation of the accessory pathway (EPS and RF ablation).
Other factors that appear to influence the risk of SCD are the presence of multiple bypass tracts, short AP refractory periods (
The cause of SCD in WPW syndrome is rapid conduction of AF to the ventricles via the AP, resulting in ventricular fibrillation (VF). AF develops in one fifth to one third of patients with WPW syndrome; the reasons for this and the effects of AP ablation on its development are unclear.
However, 1 study hypothesized that 2 mechanisms are involved in the pathogenesis of AF in patients with WPW syndrome: one is related to the AP that predisposes the atria to fibrillation, and the other is independent from the AP and is related to increased atrial vulnerability present in these individuals.[10]
According to the literature, risk factors for the development of AF in the setting of WPW syndrome include advancing age (2 peak ages for AF occurrence are recognized, one at 30 years and the other at 50 years), male gender, and prior history of syncope.[11]
Certain factors increase the likelihood of VF, including rapidly conducting APs and multiple pathways.[12] Cases have also been reported in association with esophageal studies, digoxin, and verapamil. A few reports document spontaneous VF in WPW syndrome, and SVT may degenerate into AF, thus leading to VF[13] ; however, both scenarios are rare in pediatric patients.
Morbidity may be related to rapid near syncopal or syncopal arrhythmias. Even when syncope is absent, the arrhythmia episodes may be highly symptomatic. In most patients, the SVT is well tolerated and is not life threatening. However, the potential for syncope, hemodynamically compromising rhythms, or sudden death may prevent patients with WPW syndrome from participating in competitive sports or hazardous occupations until the substrate is definitively addressed and cured by a catheter ablation procedure.
PreviousNextPatient EducationPatient education is of paramount importance in patients with WPW syndrome. This is especially true in asymptomatic young patients who have been told of their abnormal ECG results. Periodic follow-up care of such patients is necessary, along with thoughtful discussions of consideration for EPS and prophylactic catheter ablation.
Urge patients to carry a sample ECG in sinus rhythm and a medical identification bracelet in case of cardiac arrest.
Educate patients who are being treated with drug therapy thoroughly regarding the disease and the type of medications they are taking. Such patients must be taught the following:
How to recognize disease recurrenceHow to perform vagal maneuvers, when neededTo keep their follow-up appointmentsTo identify the adverse effects of antiarrhythmic drugsTo avoid competitive sportsTo learn about ablative options and the indications for ablationPatients with WPW syndrome should also educate their family members, and their siblings should be screened for preexcitation with 12-lead ECG.
For patient education resources, see the Heart Center, as well as Supraventricular Tachycardia.
PreviousProceed to Clinical Presentation  Contributor Information and DisclosuresAuthorChristopher R Ellis, MD, FACC Assistant Professor of Medicine, Cardiac Electrophysiology, Vanderbilt Heart and Vascular Institute, Vanderbilt University School of Medicine; Attending Physician, Adult Cardiovascular Medicine, Veterans Affairs Medical Center-Nashville, Tennessee Valley Healthcare System
Christopher R Ellis, MD, FACC is a member of the following medical societies: Alpha Omega Alpha, American College of Cardiology, and Heart Rhythm Society
Disclosure: Nothing to disclose.
Hugh D Allen, MD Professor, Department of Pediatrics, Division of Pediatric Cardiology and Department of Internal Medicine, Ohio State University College of Medicine
Hugh D Allen, MD is a member of the following medical societies: American Academy of Pediatrics, American College of Cardiology, American Heart Association, American Pediatric Society, American Society of Echocardiography, Society for Pediatric Research, Society of Pediatric Echocardiography, and Western Society for Pediatric Research
Disclosure: Nothing to disclose.
Charles I Berul, MD Professor of Pediatrics and Integrative Systems Biology, George Washington University School of Medicine; Chief, Division of Cardiology, Children's National Medical Center
Charles I Berul, MD is a member of the following medical societies: American Academy of Pediatrics, American College of Cardiology, American Heart Association, Cardiac Electrophysiology Society, Heart Rhythm Society, Pediatric and Congenital Electrophysiology Society, and Society for Pediatric Research
Disclosure: Johnson & Johnson Consulting fee Consulting
Robert Murray Hamilton, MD, MSc, FRCPC Section Head, Electrophysiology, Senior Associate Scientist, Physiology and Experimental Medicine, Labatt Family Heart Centre; Professor, Department of Pediatrics, University of Toronto Faculty of Medicine
Robert Murray Hamilton, MD, MSc, FRCPC is a member of the following medical societies: American Heart Association, Canadian Cardiovascular Society, Canadian Medical Association, Canadian Medical Protective Association, Cardiac Electrophysiology Society, Heart Rhythm Society, Ontario Medical Association, Pediatric Electrophysiology Society, Royal College of Physicians and Surgeons of Canada, and Society for Pediatric Research
Disclosure: Nothing to disclose.
Shubhayan Sanatani, MD Associate Professor, Department of Pediatrics, University of British Columbia Faculty of Medicine; Consulting Staff, Division of Pediatric Cardiology, British Columbia Children's Hospital, Canada
Shubhayan Sanatani, MD is a member of the following medical societies: British Columbia Medical Association, Canadian Cardiovascular Society, Canadian Heart Rhythm Society, Canadian Heart Rhythm Society, Canadian Medical Association, and Royal College of Physicians and Surgeons of Canada
Disclosure: Nothing to disclose.
Russell F Kelly MD, Assistant Professor, Department of Internal Medicine, Rush Medical College; Chairman of Adult Cardiology and Director of the Fellowship Program, Cook County Hospital
Russell F Kelly is a member of the following medical societies: American College of Cardiology
Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Medscape Salary Employment
Brian Olshansky, MD Professor of Medicine, Department of Internal Medicine, University of Iowa College of Medicine
Brian Olshansky, MD is a member of the following medical societies: American College of Cardiology, American Heart Association, Cardiac Electrophysiology Society, and Heart Rhythm Society
Disclosure: Guidant/Boston Scientific Honoraria Speaking and teaching; Medtronic Honoraria Speaking and teaching; Guidant/Boston Scientific Consulting fee Consulting; BioControl Consulting fee Consulting; Boehringer Ingelheim Consulting fee Consulting; Amarin Consulting fee Review panel membership; sanofi aventis Review panel membership
Stuart Berger, MD Professor of Pediatrics, Division of Cardiology, Medical College of Wisconsin; Chief of Pediatric Cardiology, Medical Director of Pediatric Heart Transplant Program, Medical Director of The Heart Center, Children's Hospital of Wisconsin
Stuart Berger, MD is a member of the following medical societies: American Academy of Pediatrics, American College of Cardiology, American College of Chest Physicians, American Heart Association, and Society for Cardiac Angiography and Interventions
Disclosure: Nothing to disclose.
Jeffrey N Rottman, MD Professor of Medicine and Pharmacology, Vanderbilt University School of Medicine; Chief, Department of Cardiology, Nashville Veterans Affairs Medical Center
Jeffrey N Rottman, MD is a member of the following medical societies: American Heart Association and North American Society of Pacing and Electrophysiology (NASPE)
Disclosure: Nothing to disclose.
M Silvana Horenstein, MD Assistant Professor, Department of Pediatrics, University of Texas Medical School at Houston; Medical Doctor Consultant, Legacy Department, Best Doctors, Inc
M Silvana Horenstein, MD is a member of the following medical societies: American Academy of Pediatrics, American College of Cardiology, and American Medical Association
Disclosure: Nothing to disclose.
ReferencesWolff, L., Parkinson, J., White, PD. Bundle-branch block with short P-R interval in healthy young people prone to paroxysmal tachycardia. American Heart Journal. 1930/08;5:685-704.
Durrer D, Schuilenburg RM, Wellens HJ. Pre-excitation revisited. Am J Cardiol. Jun 1970;25(6):690-7. [Medline].
Calkins H, Sousa J, el-Atassi R, et al. Diagnosis and cure of the Wolff-Parkinson-White syndrome or paroxysmal supraventricular tachycardias during a single electrophysiologic test. N Engl J Med. Jun 6 1991;324(23):1612-8. [Medline].
Pappone C, Vicedomini G, Manguso F, et al. Risk of malignant arrhythmias in initially symptomatic patients with wolff-Parkinson-white syndrome: results of a prospective long-term electrophysiological follow-up study. Circulation. Feb 7 2012;125(5):661-8. [Medline].
Pappone C, Santinelli V, Manguso F, Augello G, Santinelli O, Vicedomini G. A randomized study of prophylactic catheter ablation in asymptomatic patients with the Wolff-Parkinson-White syndrome. N Engl J Med. Nov 6 2003;349(19):1803-11. [Medline].
Sethi KK, Dhall A, Chadha DS, Garg S, Malani SK, Mathew OP. WPW and preexcitation syndromes. J Assoc Physicians India. Apr 2007;55 Suppl:10-5. [Medline].
Ehtisham J, Watkins H. Is Wolff-Parkinson-White syndrome a genetic disease?. J Cardiovasc Electrophysiol. Nov 2005;16(11):1258-62. [Medline].
Gollob MH, Green MS, Tang AS, Gollob T, Karibe A, Ali Hassan AS. Identification of a gene responsible for familial Wolff-Parkinson-White syndrome. N Engl J Med. Jun 14 2001;344(24):1823-31. [Medline].
Brembilla-Perrot B, Yangni N'da O, Huttin O, Chometon F, Groben L, Christophe C. Wolff-Parkinson-White syndrome in the elderly: clinical and electrophysiological findings. Arch Cardiovasc Dis. Jan 2008;101(1):18-22. [Medline].
Zhang Y, Wang L. Atrial vulnerability is a major mechanism of paroxysmal atrial fibrillation in patients with Wolff-Parkinson-White syndrome. Med Hypotheses. 2006;67(6):1345-7. [Medline].
Szumowski L, Walczak F, Urbanek P, Szufladowicz E, Ratajska E, Kepski R, et al. Risk factors of atrial fibrillation in patients with Wolff-Parkinson-White syndrome. Kardiol Pol. Mar 2004;60(3):206-16; discussion 217. [Medline].
Bromberg BI, Lindsay BD, Cain ME, Cox JL. Impact of clinical history and electrophysiologic characterization of accessory pathways on management strategies to reduce sudden death among children with Wolff-Parkinson-White syndrome. J Am Coll Cardiol. Mar 1 1996;27(3):690-5. [Medline].
Attoyan C, Haissaguerre M, Dartigues JF, Le Métayer P, Warin JF, Clémenty J. [Ventricular fibrillation in Wolff-Parkinson-White syndrome. Predictive factors]. Arch Mal Coeur Vaiss. Jul 1994;87(7):889-97. [Medline].
Mark DG, Brady WJ, Pines JM. Preexcitation syndromes: diagnostic consideration in the ED. Am J Emerg Med. Sep 2009;27(7):878-88. [Medline].
Fengler BT, Brady WJ, Plautz CU. Atrial fibrillation in the Wolff-Parkinson-White syndrome: ECG recognition and treatment in the ED. Am J Emerg Med. Jun 2007;25(5):576-83. [Medline].
Arruda, Mauricio S., et al. Development and validation of an ECG algorithm for identifying accessory pathway ablation site in Wolff-Parkinson-White syndrome. Journal of Cardiovascular Electrophysiology. 1998/01;9:2-12.
Burnes JE, Taccardi B, Rudy Y. A noninvasive imaging modality for cardiac arrhythmias. Circulation. Oct 24 2000;102(17):2152-8. [Medline]. [Full Text].
Ghosh S, Avari JN, Rhee EK, Woodard PK, Rudy Y. Hypertrophic cardiomyopathy with preexcitation: insights from noninvasive electrocardiographic imaging (ECGI) and catheter mapping. J Cardiovasc Electrophysiol. Nov 2008;19(11):1215-7. [Medline]. [Full Text].
Pappone C, Manguso F, Santinelli R, Vicedomini G, Sala S, Paglino G. Radiofrequency ablation in children with asymptomatic Wolff-Parkinson-White syndrome. N Engl J Med. Sep 16 2004;351(12):1197-205. [Medline].
Sarubbi B, D'Alto M, Vergara P, Calvanese R, Mercurio B, Russo MG, et al. Electrophysiological evaluation of asymptomatic ventricular pre-excitation in children and adolescents. Int J Cardiol. Feb 15 2005;98(2):207-14. [Medline].
Duszanska A, Lenarczyk R, Kowalski O, Streb W, Kukulski T, Kalarus Z. Evaluation of left ventricular systolic and diastolic function in patients with atrioventricular re-entrant tachycardia treated by radiofrequency current ablation. Acta Cardiol. Apr 2008;63(2):221-7. [Medline].
Jackman WM, Wang XZ, Friday KJ, et al. Catheter ablation of accessory atrioventricular pathways (Wolff- Parkinson-White syndrome) by radiofrequency current. N Engl J Med. Jun 6 1991;324(23):1605-11. [Medline].
Pappone C, Radinovic A, Santinelli V. Sudden death and ventricular preexcitation: is it necessary to treat the asymptomatic patients?. Curr Pharm Des. 2008;14(8):762-5. [Medline].
Gulletta S, Tsiachris D, Radinovic A, Bisceglia C, et al. Safety and Efficacy of Open Irrigated-Tip Catheter Ablation of Wolff-Parkinson-White Syndrome in Children and Adolescents. Pacing Clin Electrophysiol. Jan 28 2013;[Medline].
Â
 Classic Wolff-Parkinson-White electrocardiogram with short PR, QRS >120 ms, and delta wave. Preexcited atrial fibrillation. Variants of Wolff-Parkinson-White syndrome (unusual accessory pathways). Accessory pathway potential and local AV fusion at successful RF ablation site with loss of preexcitation and return of normal HV interval. Electrocardiogram of asymptomatic 17-year-old male who was incidentally discovered to have Wolff-Parkinson-White pattern. It shows sinus rhythm with evident preexcitation. To locate accessory pathway (AP), initial 40 ms of QRS (delta wave) is evaluated. Note that delta wave is positive in I and aVL, negative in III and aVF, isoelectric in V1, and positive in rest of precordial leads. Therefore, this is likely posteroseptal AP. 12-lead electrocardiogram from asymptomatic 7-year-old boy with Wolff-Parkinson-White pattern. Delta waves are positive in I and aVL; negative in II, III, and aVF; isoelectric in V1; and positive in rest of precordial leads. This predicts posteroseptal location for accessory pathway. 12-lead electrocardiogram showing short PR interval and delta waves consistent with presence of accessory pathway.
Classic Wolff-Parkinson-White electrocardiogram with short PR, QRS >120 ms, and delta wave. Preexcited atrial fibrillation. Variants of Wolff-Parkinson-White syndrome (unusual accessory pathways). Accessory pathway potential and local AV fusion at successful RF ablation site with loss of preexcitation and return of normal HV interval. Electrocardiogram of asymptomatic 17-year-old male who was incidentally discovered to have Wolff-Parkinson-White pattern. It shows sinus rhythm with evident preexcitation. To locate accessory pathway (AP), initial 40 ms of QRS (delta wave) is evaluated. Note that delta wave is positive in I and aVL, negative in III and aVF, isoelectric in V1, and positive in rest of precordial leads. Therefore, this is likely posteroseptal AP. 12-lead electrocardiogram from asymptomatic 7-year-old boy with Wolff-Parkinson-White pattern. Delta waves are positive in I and aVL; negative in II, III, and aVF; isoelectric in V1; and positive in rest of precordial leads. This predicts posteroseptal location for accessory pathway. 12-lead electrocardiogram showing short PR interval and delta waves consistent with presence of accessory pathway. 
  View Table List Read more about Wolff-Parkinson-White Syndrome on MedscapeRelated Reference Topics
 View Table List Read more about Wolff-Parkinson-White Syndrome on MedscapeRelated Reference TopicsLown-Ganong-Levine Syndrome
Surgical Approach to Corrected Transposition of the Great Arteries
Pediatric Ventricular Fibrillation
Related News and Articles
Consensus Statement Supports Screening Asymptomatic Young Patients With WPW Patterns
Pathologic Thoracic Spine Fracture in Presence of Parkinson's Disease and Diffuse Ankylosis
Comparison of Gait in Progressive Supranuclear Palsy, Parkinson's Disease and Healthy Older Adults
Medscape Reference © 2011 WebMD, LLC, Wolff-Parkinson-White Syndrome






0 comments:
Post a Comment